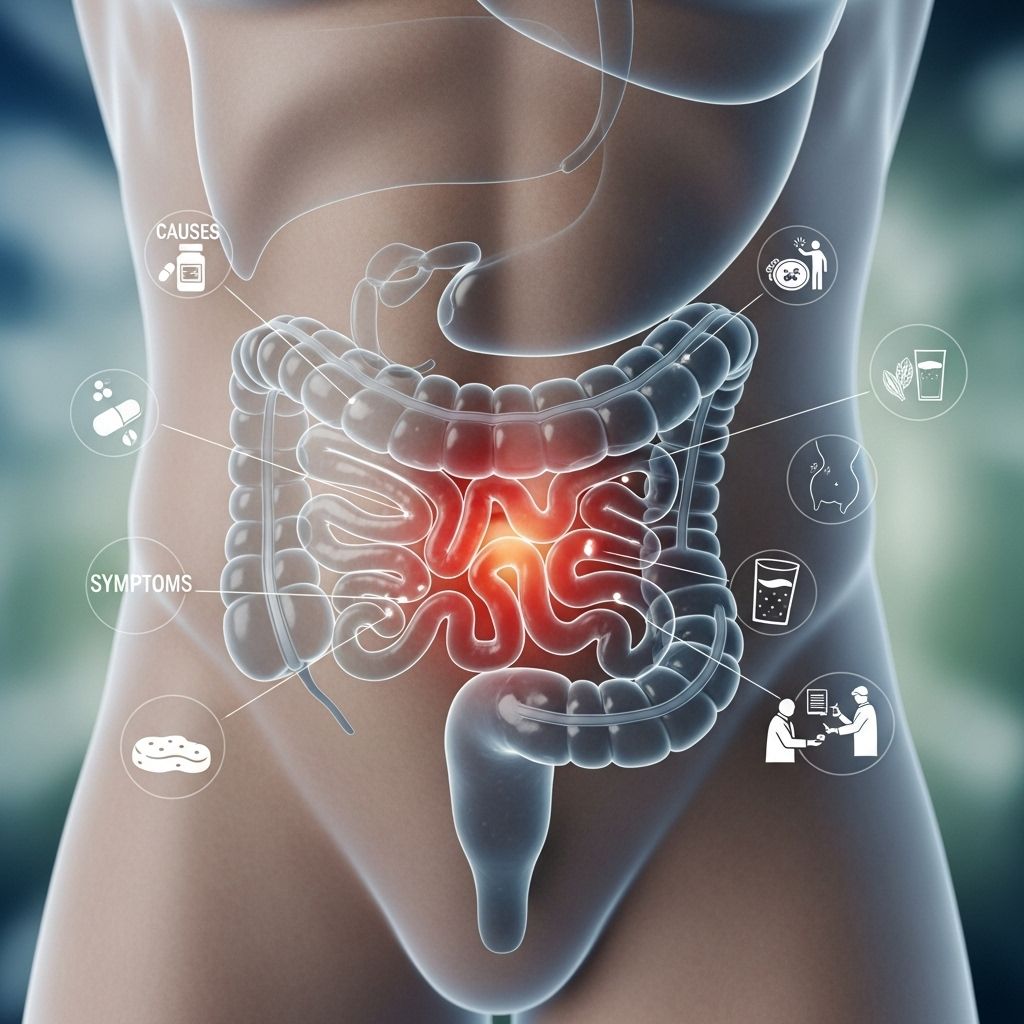
Chronic Constipation: Causes, Symptoms & Treatment Guide
Understanding and managing chronic constipation for better digestive health
Chronic constipation affects millions of people worldwide, significantly impacting quality of life and daily functioning. This common gastrointestinal condition goes beyond occasional digestive discomfort, persisting for weeks, months, or even years. Understanding the complexities of chronic constipation is essential for effective management and achieving lasting relief.
Understanding Chronic Constipation
Chronic constipation represents a persistent problem with passing stool that extends beyond temporary digestive issues. While bowel movement frequency varies naturally from person to person, with some individuals having multiple bowel movements daily and others just a few times weekly, chronic constipation specifically refers to experiencing constipation symptoms for three months or longer. This condition involves more than just infrequent bowel movements; it encompasses a range of uncomfortable symptoms that can significantly affect daily life.
The medical definition of chronic constipation follows specific diagnostic criteria. According to established medical guidelines, chronic constipation is characterized by the presence of symptoms for at least three months, with symptom onset occurring at least six months prior to diagnosis. This timeline helps distinguish chronic constipation from temporary digestive disturbances caused by dietary changes, travel, or short-term illness.
The prevalence of chronic constipation is remarkably high, affecting approximately 15% of all adults and reaching up to 30% in individuals over age 60. Some studies suggest prevalence rates ranging from 2% to 28% across different populations, with up to 63 million people in North America meeting diagnostic criteria for this condition. The condition disproportionately affects certain demographics, being more prevalent in women, older adults, and institutionalized elderly individuals.
Recognizing the Symptoms
Identifying chronic constipation requires understanding its diverse symptom profile. The condition manifests through multiple indicators, with diagnosis typically requiring at least two of six key symptoms occurring in more than 25% of bowel movements. These symptoms paint a comprehensive picture of the challenges faced by individuals with chronic constipation.
Infrequent bowel movements represent the most recognized symptom, specifically defined as having fewer than three spontaneous bowel movements per week. However, frequency alone doesn’t tell the complete story. Many individuals with chronic constipation experience straining during defecation, requiring significant effort to pass stool even when the urge is present.
The characteristics of stool itself provide important diagnostic clues. People with chronic constipation typically produce lumpy or hard stools that are difficult and painful to pass. This hardness results from prolonged transit time through the colon, allowing excessive water absorption from the stool.
Beyond physical stool characteristics, individuals often report a sensation of incomplete evacuation, feeling that the bowels haven’t fully emptied even after a bowel movement. Similarly, many experience a sensation of anorectal obstruction or blockage, feeling as though something is blocking the passage of stool. Some people resort to manual maneuvers to facilitate evacuation, using digital stimulation or support to help pass stool.
Additional symptoms may include bleeding from hemorrhoids or anal fissures caused by straining and passing hard stools. The cumulative effect of these symptoms often leads to significant discomfort, anxiety about bowel movements, and reduced quality of life.
Underlying Causes and Risk Factors
Chronic constipation develops through various mechanisms, each affecting the digestive process differently. Understanding these causes helps guide appropriate treatment strategies and identify potentially modifiable risk factors.
Primary Mechanisms
The fundamental problem in chronic constipation involves stool moving too slowly through the large intestine. This prolonged transit time allows the body to absorb excessive water from the stool, resulting in hard, dry bowel movements that are difficult to pass. Two primary colonic problems contribute to this issue: ineffective propulsion of stool through the colon and difficulty passing stool once it reaches the rectum.
The most common cause of chronic constipation is evacuation disorder, also known as pelvic floor dysfunction. This condition stems from poor bowel training or habits that prevent the pelvic floor muscles from relaxing properly during defecation. In dyssynergic defecation, there’s ineffective coordination between the pelvic floor, abdominal, rectal, and anal sphincter muscles during the evacuation process.
Lifestyle Factors
Daily habits and lifestyle choices play a crucial role in bowel function. Inadequate fluid intake reduces the water content of stool, contributing to hardness and difficult passage. Similarly, insufficient dietary fiber deprives the digestive system of the bulk needed for regular bowel movements and proper stool consistency.
Physical inactivity significantly impacts bowel function, as exercise helps stimulate intestinal motility. Changes in routine, such as travel or schedule disruptions, can temporarily throw off normal bowel patterns and potentially lead to chronic issues if not addressed. Psychological factors including stress and depression can alter gut function through the gut-brain connection. Additionally, habitually ignoring the urge to have a bowel movement can lead to diminished sensitivity to bowel signals over time.
Medical Conditions
Numerous medical conditions can contribute to or cause chronic constipation. Hypothyroidism, or underactive thyroid, slows metabolic processes throughout the body, including digestive function. Various neurological conditions affecting nerve signals to the intestines can disrupt normal bowel function. Eating disorders often involve dietary restrictions and psychological factors that impact digestion.
In women, hormonal changes during menstruation, pregnancy, and menopause can affect bowel regularity. Almost any medical condition can potentially alter bowel movements, making it important to consider overall health status when evaluating chronic constipation.
Medications
Constipation ranks among the most common medication side effects. Several drug categories frequently cause or exacerbate constipation. Allergy medications, particularly antihistamines, can slow intestinal motility. Various antidepressants affect neurotransmitters that influence gut function. Anti-seizure medications and blood pressure medications, especially calcium channel blockers, commonly cause constipation. Pain relievers, particularly opioid medications, are notorious for causing severe constipation by slowing intestinal movement.
Types of Functional Constipation
When constipation isn’t caused by secondary factors like medications or medical conditions, it’s classified as functional constipation. This category encompasses three main types, each with distinct characteristics and treatment implications.
Normal-transit constipation represents a paradoxical situation where stool passes through the colon at a normal rate and bowel movement frequency falls within normal ranges, yet patients perceive themselves as constipated. Changes in colonic water content may contribute to this perception, along with heightened sensitivity to normal bowel sensations.
Slow-transit constipation involves genuinely delayed passage of stool through the colon. This type results from impaired colonic motility, where the muscular contractions that propel stool forward occur less frequently or with reduced strength. People with slow-transit constipation often have fewer bowel movements and may not respond well to fiber supplementation alone.
Defecatory disorders involve mechanical or functional problems with the evacuation process itself. These disorders include rectal prolapse, where rectal tissue protrudes through the anal opening, and rectocele, an outpouching of the rectum. Dyssynergic defecation, the most common defecatory disorder, involves paradoxical contraction or inadequate relaxation of the pelvic floor muscles during attempted defecation.
Diagnostic Approaches
Accurate diagnosis of chronic constipation begins with a thorough evaluation of symptoms, medical history, and potential contributing factors. The diagnostic process helps distinguish constipation from other conditions and identifies the underlying type and cause.
Initial evaluation involves assessing whether symptoms meet formal diagnostic criteria. Patients must exhibit at least two of the six cardinal symptoms occurring in more than 25% of bowel movements over a three-month period. Healthcare providers carefully distinguish functional constipation from irritable bowel syndrome with constipation, where abdominal pain represents a more predominant feature.
For individuals over age 50 or those with concerning symptoms, additional testing may be necessary to rule out serious underlying conditions such as colon cancer or structural abnormalities. This evaluation might include colonoscopy or imaging studies to visualize the colon and rectum.
When basic evaluation doesn’t reveal the cause, specialized testing can identify specific constipation subtypes. Colonic transit studies measure how quickly material moves through the colon, helping distinguish slow-transit from normal-transit constipation. Anorectal manometry and balloon expulsion tests assess pelvic floor function and coordination during defecation, identifying defecatory disorders that require targeted therapy.
Treatment Strategies and Management
Managing chronic constipation requires a comprehensive, individualized approach that addresses underlying causes while providing symptom relief. Treatment typically follows a stepwise progression, beginning with conservative measures and advancing to more specialized interventions when necessary.
Lifestyle Modifications
First-line treatment focuses on optimizing lifestyle factors that influence bowel function. Adequate hydration is essential, as sufficient fluid intake helps maintain stool softness. Most adults should aim for at least eight glasses of water daily, though individual needs vary based on activity level, climate, and overall health.
Dietary fiber supplementation represents a cornerstone of constipation management. Fiber helps retain water in the stool, making it softer and easier to pass while adding bulk that stimulates intestinal contractions. Adults should gradually increase fiber intake to 25-35 grams daily through food sources or supplements. However, rapid fiber increases can cause bloating and gas, so gradual implementation is important.
Regular physical activity stimulates intestinal motility and supports overall digestive health. Even moderate exercise like daily walking can significantly improve bowel function. Establishing a regular toilet routine, particularly responding promptly to bowel urges and allowing adequate time for unhurried defecation, helps retrain the bowel and pelvic floor muscles.
Pharmacological Treatments
When lifestyle modifications prove insufficient, various medications can provide relief. Osmotic laxatives work by drawing water into the colon, softening stool and stimulating bowel movements. These agents, including polyethylene glycol, lactulose, and magnesium-based products, generally have favorable safety profiles for long-term use and represent a primary pharmacological approach.
Stimulant laxatives directly activate intestinal contractions, promoting bowel movements. While effective, these medications are typically reserved for short-term use or intermittent dosing due to concerns about dependency and potential side effects with prolonged use.
Stool softeners help prevent hard, dry stools by increasing water content, though they’re generally less effective than osmotic laxatives for chronic constipation. Lubricant laxatives coat the stool to ease passage but are also considered less effective for chronic management.
Several newer prescription medications target specific mechanisms underlying chronic constipation. Secretagogues increase fluid secretion into the intestines, while prokinetic agents enhance intestinal motility. These medications may benefit patients who don’t respond adequately to traditional treatments, particularly those with slow-transit constipation.
Specialized Therapies
Patients with defecatory disorders often benefit from pelvic floor physical therapy and biofeedback training. These approaches teach proper coordination of pelvic floor muscles during defecation, addressing the fundamental dysfunction in dyssynergic defecation. Success rates with biofeedback therapy can be substantial when properly applied to appropriate patients.
For individuals with medication-induced constipation, switching medications or adjusting dosages, when medically appropriate, may significantly improve symptoms. This approach requires careful coordination with prescribing physicians to ensure that underlying conditions remain adequately treated.
Surgical Interventions
Surgery for chronic constipation is reserved for carefully selected patients whose symptoms persist despite maximal medical therapy. Surgical options address specific anatomical problems or, in severe cases of slow-transit constipation unresponsive to all other treatments, may involve colonic resection. Given the irreversible nature and potential complications of surgical interventions, thorough preoperative evaluation and discussion of risks versus benefits is essential.
Living with Chronic Constipation
Chronic constipation significantly impacts quality of life, affecting physical comfort, emotional well-being, and daily activities. The condition is associated with increased healthcare utilization, including frequent physician visits, diagnostic procedures, and medication costs. Beyond direct medical impact, chronic constipation can cause anxiety, social limitations, and reduced productivity.
Managing chronic constipation successfully requires patience, persistence, and often a combination of treatment approaches. Many individuals need to experiment with different strategies to find what works best for their specific situation. Working closely with healthcare providers to develop a personalized management plan optimizes outcomes and improves quality of life.
The association between chronic constipation and factors like lower socioeconomic status, reduced physical activity, and stressful life events highlights the importance of addressing overall lifestyle and well-being. Support from healthcare providers, family members, and potentially support groups can help individuals cope with the challenges of chronic constipation and maintain motivation for ongoing management.
Frequently Asked Questions
Q: How is chronic constipation different from occasional constipation?
A: Chronic constipation persists for three months or longer with symptom onset at least six months before diagnosis, whereas occasional constipation is temporary and typically resolves within days or weeks with simple interventions.
Q: Can chronic constipation be cured completely?
A: While chronic constipation can often be effectively managed with appropriate treatment, whether it can be completely cured depends on the underlying cause. Addressing secondary causes like medications or medical conditions may resolve constipation, while functional constipation typically requires ongoing management strategies.
Q: When should I see a doctor about constipation?
A: You should consult a healthcare provider if constipation persists for more than three weeks, if you’re over 50 with new-onset constipation, if you experience severe abdominal pain or rectal bleeding, or if constipation significantly impacts your quality of life despite self-care measures.
Q: Are fiber supplements safe for long-term use?
A: Yes, fiber supplements are generally safe for long-term use when taken with adequate fluids. However, they should be introduced gradually to minimize gas and bloating, and the dosage should be adjusted based on individual response and tolerance.
Q: Why is chronic constipation more common in women?
A: Multiple factors contribute to higher constipation rates in women, including hormonal fluctuations affecting intestinal motility, anatomical differences in pelvic floor structure, and higher rates of conditions like hypothyroidism that can cause constipation. Pregnancy and childbirth can also impact pelvic floor function.
Q: Can stress cause chronic constipation?
A: Yes, stress can contribute to chronic constipation through the gut-brain connection. Stress affects digestive motility, muscle tension, and bowel habits. Managing stress through relaxation techniques, exercise, and other coping strategies may help improve bowel function.
Q: What’s the difference between constipation and irritable bowel syndrome?
A: The main distinguishing feature is that irritable bowel syndrome includes abdominal pain as a predominant symptom, along with altered bowel habits. Functional constipation focuses primarily on difficulty with bowel movements without the significant abdominal pain characteristic of IBS.
Q: Do I need to take laxatives forever if I have chronic constipation?
A: Not necessarily. Many people can manage chronic constipation through lifestyle modifications alone. When medications are needed, some individuals require long-term use while others may eventually reduce or discontinue them once bowel function improves. The approach should be individualized based on response to treatment and underlying causes.
Read full bio of Sneha Tete











