Carotid Artery Disease: Symptoms and Causes Explained
Understanding carotid artery disease: risk factors, warning signs, causes, and the importance of early detection and prevention.
Carotid Artery Disease: Symptoms and Causes
Carotid artery disease is a chronic vascular condition characterized by the accumulation of fatty deposits in the carotid arteries, the main vessels that carry blood to the brain and head.
As these arteries become narrowed or blocked over time, the risk of stroke rises significantly. Because the disease often progresses without noticeable symptoms, understanding its causes, recognizing potential warning signs, and knowing when to seek medical care is vital for prevention and early treatment.
Overview
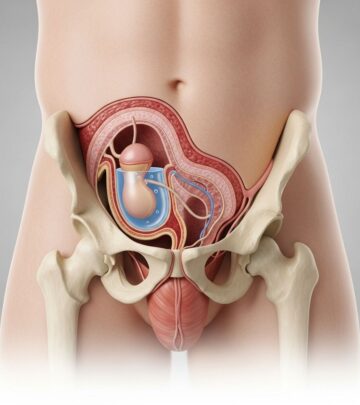
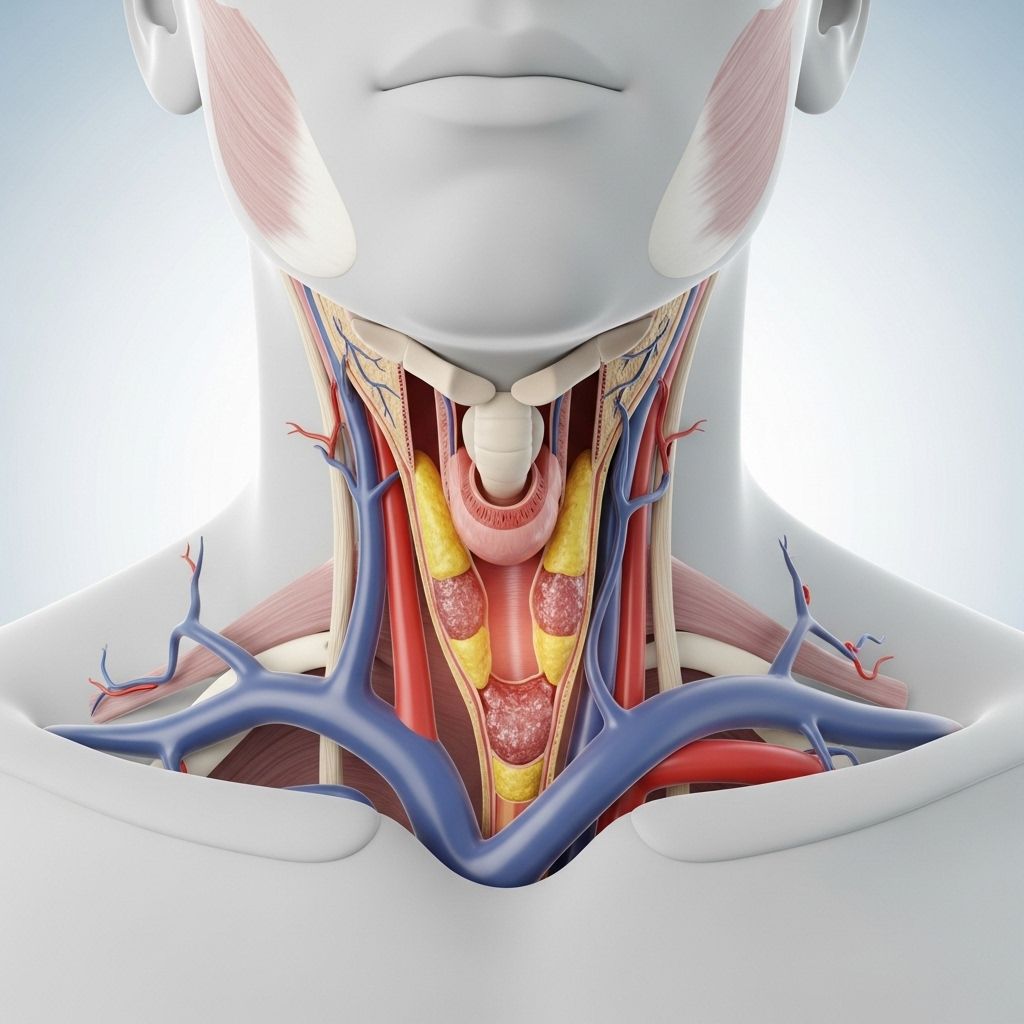
The carotid arteries are a pair of large blood vessels, one on each side of the neck, responsible for supplying oxygen-rich blood to the brain and head.Carotid artery disease (carotid stenosis) occurs when plaques made of cholesterol, calcium, and fibrous tissue gradually build up within these arteries. This process, known as atherosclerosis, can eventually restrict or block blood flow to the brain.
When blood flow is partially or fully blocked, it increases the risk of a stroke. Stroke happens when the brain loses its blood supply, depriving brain cells of oxygen and starting cell death within minutes. Stroke is one of the leading causes of death and long-term disability in adults worldwide.
Key Points
- Carotid artery disease remains a leading cause of stroke.
- The disease often develops slowly and silently, with many individuals not realizing they have it until a stroke or transient ischemic attack (TIA) occurs.
- Treatment combines lifestyle changes, medications, and sometimes surgical interventions.
The Carotid Arteries: Vital Blood Vessels
The carotid arteries are located on each side of the neck. Each artery splits into two main branches:
- Internal carotid artery: Supplies blood to the brain.
- External carotid artery: Supplies blood to the face and neck.
Because these arteries are the primary pathway for blood to reach the brain, any narrowing or obstruction dramatically raises the risk of neurological complications.
Symptoms
In its early stages, carotid artery disease commonly produces no symptoms. Many people are unaware of the disease until it has advanced enough to reduce blood flow to the brain and cause a TIA or stroke.
Warning Signs: Stroke and TIA Symptoms
Even advanced carotid artery disease may only become obvious when a stroke or TIA occurs. Key symptoms include:
- Sudden numbness or weakness in the face or limbs, often on only one side of the body
- Sudden trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden dizziness or loss of balance and coordination
- Sudden, severe headache with no known cause
These symptoms can last from a few minutes to several hours, or in the case of stroke, can result in permanent impairment or death.
Transient Ischemic Attack (TIA)
A TIA, or “mini-stroke,” is a temporary disruption in blood flow to the brain, producing stroke-like symptoms that resolve within 24 hours and usually do not cause permanent damage. However, a TIA is a major warning sign — individuals who have experienced a TIA are at much higher risk of suffering a full stroke in the future.
When to Seek Medical Help
- Call emergency services immediately if you or someone you know exhibits any symptoms of stroke, even if they resolve quickly. Immediate treatment is critical to preventing permanent brain damage and disability.
- If you have known risk factors for carotid artery disease or concerns about your health, consult a healthcare provider even in the absence of symptoms. Proactive management can help reduce your risk of a disabling or fatal stroke.
Causes
The most common cause of carotid artery disease is atherosclerosis — the gradual accumulation of fatty deposits (plaques) inside the artery walls. Over time, these plaques can:
- Narrow the artery, reducing the amount of blood able to reach the brain.
- Rupture, causing blood clots that can travel to the brain and block smaller blood vessels.
Carotid artery disease shares many similarities with other forms of arterial disease, such as coronary artery disease (heart arteries) and peripheral artery disease (leg arteries).
Pathway of the Disease
- Cholesterol and other lipids accumulate in patches within the artery wall.
- Calcification and fibrous tissue make plaques harder and more likely to rupture.
- Blood flow to the brain becomes progressively limited.
- A sudden rupture or blood clot can block blood flow completely, causing a stroke.
Risk Factors
Several risk factors increase the likelihood of developing carotid artery disease — most are the same as for other cardiovascular diseases. Key risk factors include:
- High blood pressure (hypertension): Puts additional strain on artery walls, accelerating damage.
- High cholesterol: Facilitates plaque formation within arteries.
- Diabetes: Damages arteries and accelerates atherosclerosis.
- Smoking: Directly injures blood vessels and promotes arterial damage.
- Obesity or being overweight
- Physical inactivity
- Unhealthy diet: Especially diets high in saturated fat, trans fat, and cholesterol.
- Family history of atherosclerosis, carotid artery disease, or early strokes.
- Age: Risk increases with age; carotid stenosis is particularly common in adults over 75.
Less Common Risk Factors
- Sleep apnea
- Chronic inflammatory conditions (such as lupus or rheumatoid arthritis)
- High levels of homocysteine: An amino acid in the blood associated with increased arterial risk
Complications
The main complication of carotid artery disease is ischemic stroke — caused by an abrupt reduction or total loss of blood flow to part of the brain. Carotid artery disease can also lead to:
- Transient Ischemic Attacks (TIAs) — short-lived, mini-strokes indicating significantly increased stroke risk.
- Silent (asymptomatic) strokes — strokes that may not have immediate symptoms but can progressively damage cognitive or motor function.
Prevention
- Control blood pressure and cholesterol levels with medication and lifestyle changes as needed.
- Stop smoking. This is one of the most critical steps for vascular health.
- Manage diabetes carefully to slow disease progression.
- Eat a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Engage in regular physical activity — at least 150 minutes of moderate exercise per week for most adults.
- Maintain a healthy weight.
- Attend regular checkups for blood pressure, cholesterol, and vascular health screening.
Diagnosis and Prognosis
Carotid artery disease is sometimes discovered during routine physical exams when a doctor detects a bruit — a swooshing sound in the neck arteries that may indicate turbulent blood flow due to narrowing.
Further diagnostic procedures may include:
- Ultrasound imaging of the carotid arteries (Doppler study)
- CT angiography or Magnetic Resonance Angiography (MRA)
- Blood tests for cholesterol, blood sugar, and other markers
Early detection allows timely intervention, dramatically reducing the risk of stroke and disabling complications.
Current Treatment Approaches
Treatment for carotid artery disease focuses on reducing stroke risk. Options include:
- Lifestyle changes such as diet, exercise, and quitting smoking
- Medications to control blood pressure, cholesterol, and sometimes blood-thinning drugs to prevent clot formation
- Surgical procedures or angioplasty with stenting in certain cases to open narrowed arteries
The precise treatment plan depends on the degree of narrowing, overall health status, and the presence or absence of symptoms.
Frequently Asked Questions (FAQs)
What are the carotid arteries and why are they important?
The carotid arteries are two major blood vessels in the neck that carry oxygen-rich blood to the brain and head. Their health is crucial because any blockage can severely impact brain function and increase stroke risk.
Is carotid artery disease always symptomatic?
No. In most cases, carotid artery disease develops without causing symptoms. Many individuals only discover they have it after a TIA or stroke has occurred.
What puts me at risk for developing carotid artery disease?
Major risk factors include high blood pressure, high cholesterol, diabetes, smoking, aging, inactivity, and having a family history of cardiovascular disease.
How is carotid artery disease diagnosed?
Diagnosis usually starts with a physical examination (listening for a bruit), followed by imaging studies like a carotid ultrasound, CT angiography, or MRA, along with laboratory testing of cholesterol and blood sugar levels.
How can I reduce my risk of stroke from carotid artery disease?
Managing blood pressure, cholesterol, diabetes, and adopting a healthy lifestyle—quit smoking, exercise, and eat well—significantly lower the risk. For advanced cases, your healthcare provider may recommend medication or surgical interventions.
If I have a TIA, what should I do?
A TIA is a warning sign of a possible future stroke. Seek immediate emergency medical attention, even if symptoms resolve quickly.
Summary Table: Carotid Artery Disease At-a-Glance
| Aspect | Details |
|---|---|
| Definition | Narrowing/obstruction of carotid arteries by plaques |
| Key Risk | Stroke |
| Symptoms | Usually none until TIA or stroke; sudden weakness, vision trouble, speech difficulty, dizziness, severe headache |
| Main Causes | Atherosclerosis (lipid, cholesterol, and calcium deposits) |
| Major Risk Factors | Hypertension, high cholesterol, diabetes, smoking, age, inactivity |
| Diagnosis | Physical exam, ultrasound, CT/MRA imaging, blood tests |
| Treatment | Lifestyle changes, medications, surgical or catheter procedures |
| Prevention | Risk control, early detection, healthy living |
Conclusion
Carotid artery disease is a progressive and often silent threat to brain health, most commonly presenting with no symptoms until a TIA or devastating stroke occurs. Early recognition, risk factor management, and prompt medical care are essential in minimizing the risk of lifelong disability or premature death from this condition. Anyone with symptoms of stroke or TIA, or with multiple cardiovascular risk factors, should discuss screening and prevention strategies with their healthcare provider.
Read full bio of Sneha Tete