Costochondritis: Symptoms, Causes, and When to Seek Care
Learn about costochondritis, including its symptoms, causes, diagnosis, when to seek help, and how it differs from other conditions.
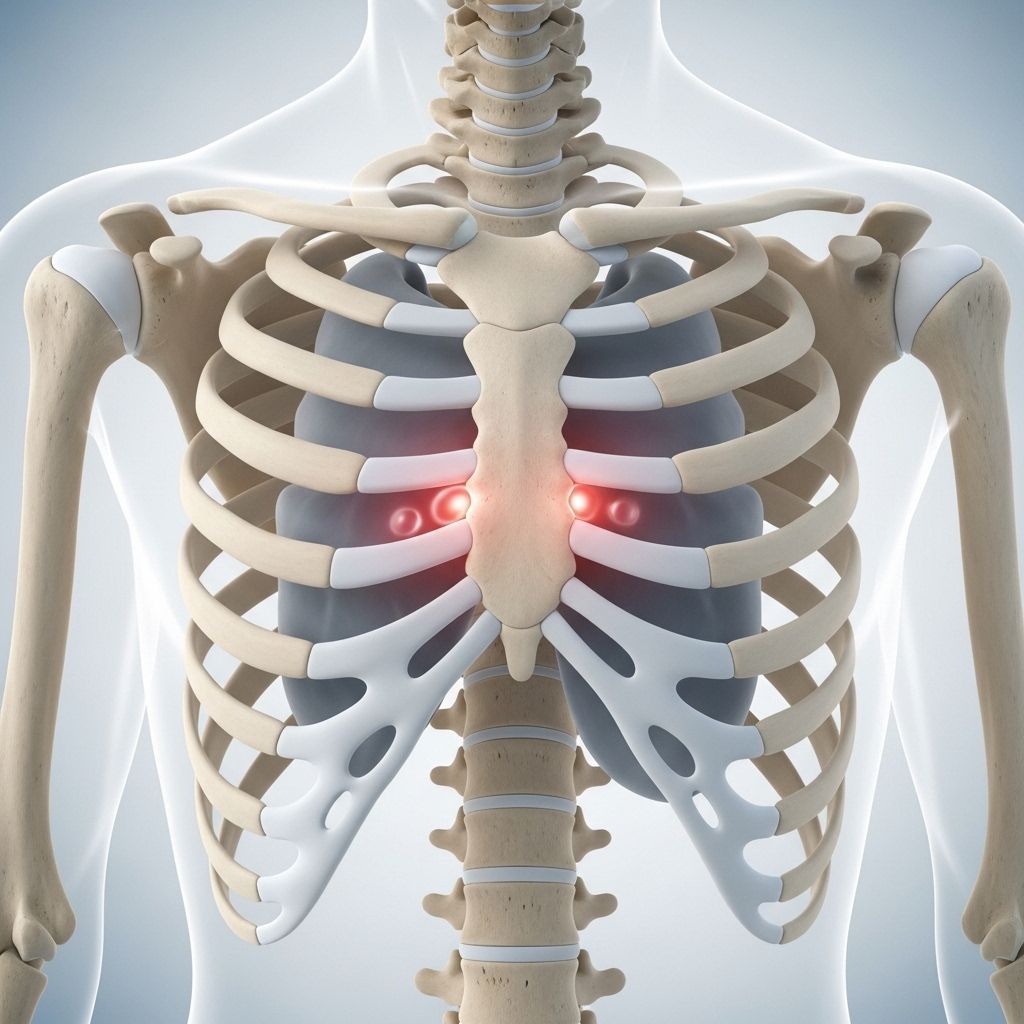
Costochondritis is a condition characterized by the inflammation of the cartilage connecting the ribs to the breastbone (sternum). While the symptoms can mimic those of heart-related conditions, costochondritis is usually a benign and self-limiting problem. Understanding its symptoms, potential causes, and when to seek medical care is crucial for effective management and peace of mind.
What Is Costochondritis?
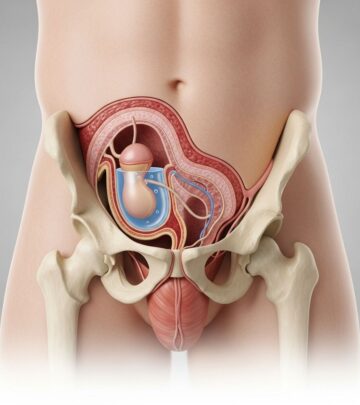
Costochondritis (pronounced kos-toe-kon-DRY-tis) is inflammation of the cartilage where the ribs attach to the sternum. This region, known as the costosternal junction, helps form the structure of the upper chest. When this cartilage becomes irritated or inflamed, it leads to localized pain and tenderness. The condition is sometimes referred to as:
- Chest wall pain syndrome
- Costosternal syndrome
- Costosternal chondrodynia
Although costochondritis can cause significant discomfort, it is not associated with life-threatening illnesses, despite often being mistaken for heart attack symptoms due to its chest pain presentation.
Symptoms of Costochondritis
The most prominent and troubling symptom is chest pain, typically localized near the attachment of the ribs to the sternum.
- Pain Location: Most commonly affects the upper ribs on the left side, but can also occur on either side of the chest.
- Pain Character: May be sharp, aching, or develop as a pressure-like sensation. The pain often worsens with certain movements or pressure.
- Pain Onset: Can start suddenly or gradually and often intensifies with activity, deep breaths, coughing, or sneezing.
| Feature | Description |
|---|---|
| Side Affected | Most often left, but can be both |
| Number of Ribs | Can affect one or more adjacent ribs (frequently ribs 2–5) |
| Pain Type | Sharp, aching, pressure, or stabbing |
| Triggers | Deep breaths, coughing, physical activity, stretching, hugging |
| Radiation | May extend to shoulder or arm |
| Effect of Pressure | Intensifies when pushing on the costosternal area |
Additional notes:
- Pain typically worsens with movement of the upper body (twisting, lifting, stretching).
- Unlike heart problems, costochondritis pain often intensifies when external pressure is applied to the chest.
- Other associated symptoms such as redness, heat, or visible swelling are uncommon and may suggest other conditions.
Duration of Symptoms
Costochondritis symptoms can last from several days to weeks, and in rare cases, persist for months before resolving without intervention.
Costochondritis vs. Tietze Syndrome
| Aspect | Costochondritis | Tietze Syndrome |
|---|---|---|
| Swelling | Rare | Common (visible swelling at pain site) |
| Ribs affected | Usually ribs 2–5, lower area | Usually 2nd or 3rd rib, upper chest |
| Age Group | Most often adults over 40, especially women | Younger adults and teenagers |
| Side affected | No strong side preference | Often one side, upper chest |
Tietze syndrome presents very similarly but is distinguished by the presence of swelling at the site of pain and typically affects a single rib, higher up on the chest. Both conditions are benign but require different considerations for diagnosis.
Causes of Costochondritis
In many cases, the exact cause of costochondritis remains unclear, making it an idiopathic (unknown origin) condition. However, several factors may contribute or trigger the inflammation:
- Repeated Minor Trauma: Activities causing microtrauma (repetitive movements, excessive workouts, heavy lifting, or sudden physical stress) to the chest wall.
- Severe Coughing or Vomiting: Persistent coughing fits or vomiting episodes stressing the rib joints.
- Infections: Rarely, bacterial or viral infections affecting the chest can lead to costochondritis.
- Inflammatory Diseases: Conditions like osteoarthritis, rheumatoid arthritis, or ankylosing spondylitis which attack joints and cartilage.
- Chest Injury: Direct trauma (blow, fall, or accident) to the chest area.
- Tumors: In rare cases, tumors (either originating in the cartilage or having metastasized from another area) can contribute to localized inflammation.
- Intravenous Drug Use: May be associated with increased risk if it leads to infections.
Who Is at Risk?
- Age and Gender: Most common in women over 40.
- Activities causing chest strain: Athletes or those suddenly increasing physical activity without proper adaptation.
- History of arthritis or joint disease: May contribute to susceptibility.
When to Seek Medical Attention
While costochondritis is usually benign, chest pain can signify life-threatening conditions. Always seek prompt medical evaluation if you experience:
- Severe chest pain, especially if new, sudden in onset, or associated with exertion
- Pain radiating to left arm, jaw, neck, or back
- Shortness of breath or trouble breathing
- Nausea or vomiting
- Profuse sweating
- Lightheadedness or dizziness
- Signs of infection: redness, heat, swelling, fever, pus at painful site
These symptoms could represent a heart attack, infection, or other life-threatening causes and should never be ignored.
Diagnosis of Costochondritis
The diagnosis of costochondritis relies on careful clinical evaluation, as there are no specific laboratory or imaging tests for confirmation.
A typical diagnostic approach includes:
- Detailed Medical History: Including when and how symptoms began, aggravating and relieving factors, and associated symptoms.
- Physical Examination: Palpation of the chest wall to localize tenderness (pain usually reproducible by pressing at the costosternal area), assessment for swelling, redness, or warmth.
- Exclusion of Other Conditions: Tests such as electrocardiogram (ECG), chest X-ray, or blood work may be recommended to rule out heart, lung, or gastrointestinal pathology, especially if symptoms are atypical or severe.
- Diagnostic Criteria: Localized pain that is reproducible with palpation in the absence of other systemic findings, and no abnormalities on other diagnostic workups, strongly suggest costochondritis.
If swelling is present, or there are features suggestive of Tietze syndrome or another systemic process, additional evaluation may be needed.
Complications
- Costochondritis rarely leads to complications or long-term consequences.
- It is sometimes associated with arthritis or other inflammatory joint diseases.
- Persistent or worsening pain should prompt re-evaluation.
Managing and Treating Costochondritis
- Pain Management: Over-the-counter pain relievers (acetaminophen, ibuprofen) are often effective.
- Rest: Reducing activities that exacerbate the pain may help symptoms resolve faster.
- Application of Heat or Ice: Warm compresses or ice packs can provide temporary relief.
- In severe cases: Prescription medications such as stronger anti-inflammatory drugs or corticosteroid injections may be considered under a physician’s guidance.
- Physical Therapy: May help in chronic or persistent cases by improving posture and strengthening chest muscles.
Most people recover spontaneously within weeks or months, though recurrence can sometimes occur.
Frequently Asked Questions (FAQs)
Is costochondritis dangerous?
No, costochondritis is generally not dangerous. However, chest pain can signal other severe issues; always consult a healthcare professional for new or persistent chest pain.
Can costochondritis mimic a heart attack?
Yes, the pain can resemble that of a heart attack. Key differences include pain worsening on palpation and with certain movements. Emergency evaluation is necessary to rule out heart disease, especially with risk factors or concerning symptoms.
How can I differentiate between costochondritis and Tietze syndrome?
Both conditions cause chest pain at the costosternal junction, but Tietze syndrome is marked by noticeable swelling and typically affects a single upper rib.
How long do symptoms last?
Symptoms may last a few days to weeks and resolve gradually. In rare cases, the discomfort can persist for several months.
Can children or teenagers get costochondritis?
Yes, although it is more common in adults over 40, children and teenagers can also develop costochondritis, particularly if they experience chest trauma or repetitive physical stress.
References
- Information synthesized from authoritative medical sources including Mayo Clinic, Cleveland Clinic, and WebMD for accuracy and clarity.
Read full bio of medha deb