Hydrocele: Comprehensive Guide to Diagnosis and Treatment
Understand diagnosis, treatment, surgical options, and aftercare for hydrocele, a common cause of scrotal swelling in males of all ages.
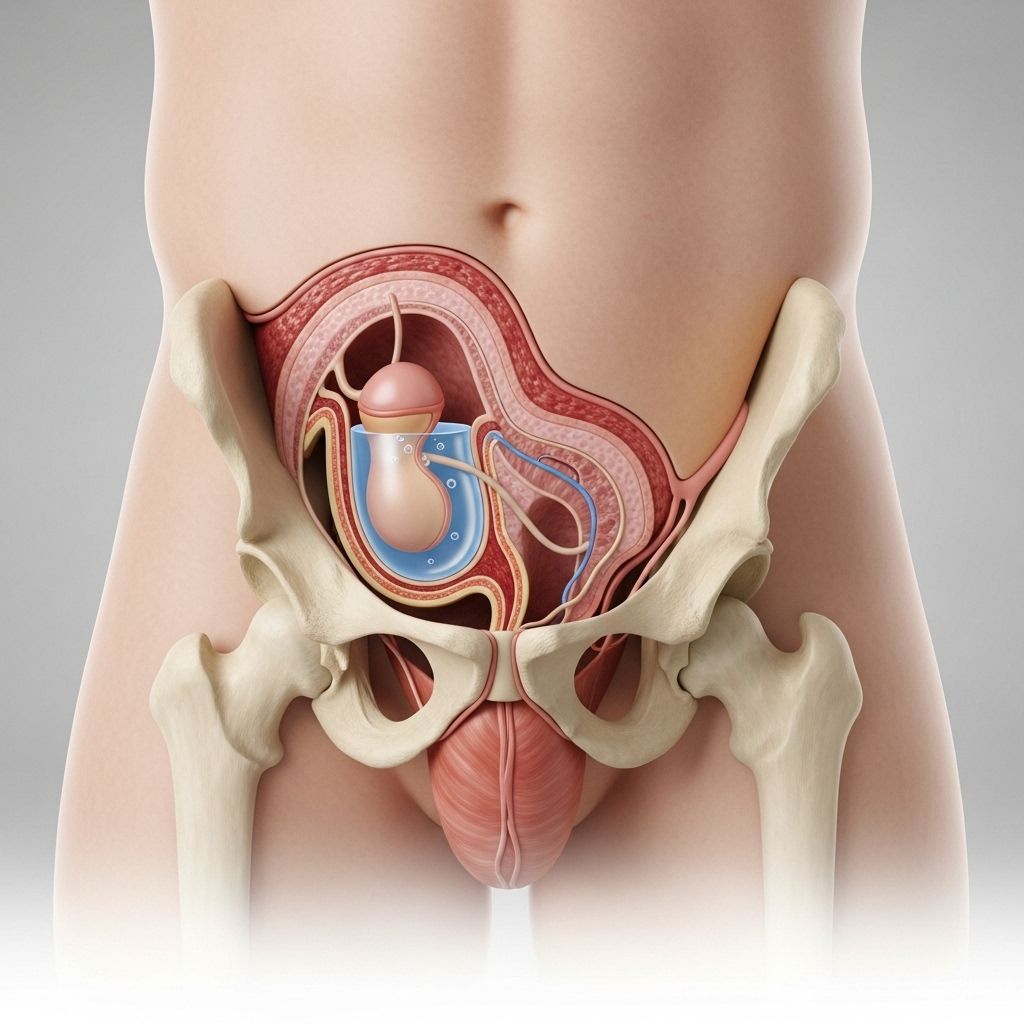
A hydrocele is a fluid-filled sac around a testicle that results in swelling of the scrotum. Hydroceles are generally painless and often harmless, but persistent or bothersome swelling warrants medical evaluation. This guide delves into diagnosis methods, treatment strategies, surgical options, and post-treatment recovery, serving as a resource for individuals and parents dealing with hydrocele concerns.
Diagnosis of Hydrocele
Early and accurate diagnosis is key to ensuring optimal care. When scrotal swelling is noticed, a thorough assessment by a healthcare provider is necessary to distinguish a hydrocele from other testicular or scrotal disorders that may require different management.
Physical Examination
A healthcare provider usually initiates diagnosis with a physical examination, including:
- Assessing the degree and location of scrotal swelling.
- Pain evaluation by gently pressing on the scrotum and abdominal region.
- Checking for signs of an inguinal hernia by pressing on the groin and scrotum; a hernia may present similarly to a hydrocele.
Transillumination Test
One distinctive exam involves shining a bright light through the scrotum (transillumination). In the case of a hydrocele:
- A clear outline of fluid surrounding the testicle will be visible as the light passes through, confirming the presence of a fluid-filled sac.
- If the testicle or swelling blocks the light, other diagnoses may be considered (such as solid masses or blood).
Additional Diagnostic Tests
When a physical examination does not provide a definitive diagnosis or if an infection or another condition is suspected, more tests may be ordered:
- Blood and urine tests: These can identify infections or inflammation, such as epididymitis, which may contribute to swelling.
- Ultrasound imaging: This non-invasive test uses high-frequency sound waves to create images of the scrotum’s internal structures. Ultrasound helps to:
- Rule out inguinal hernia, testicular tumors, or other causes of swelling.
- Locate hydroceles not easily felt during physical examination.
Treatment Options for Hydrocele
The appropriate treatment for a hydrocele depends on several factors, including the patient’s age, symptoms, hydrocele size, and underlying cause. Careful monitoring or intervention by a healthcare provider ensures a tailored approach for optimal outcomes.
Treatment in Infants and Children
- In newborns and infants, hydroceles are quite common and frequently resolve spontaneously within the first year.
- Observation is typically recommended unless:
- The swelling persists beyond one year of age, or
- The hydrocele becomes larger or is associated with discomfort or infection.
- If the hydrocele is persistent, progressively growing, or co-exists with an inguinal hernia, surgical intervention may be indicated.
Treatment in Adults
- In adult males, hydroceles often resolve on their own, particularly if secondary to minor trauma or inflammation.
- Observation without active treatment is suitable if the hydrocele is small, painless, and not causing embarrassment or interference with activities.
- Surgical removal, or hydrocelectomy, is generally reserved for cases with:
- Significant discomfort,
- Scrotal size that interferes with daily life, or
- Cosmetic concerns.
- Large or persistent hydroceles, especially if unresponsive to conservative measures, are candidates for surgery.
Hydrocele Surgery: Hydrocelectomy
If a hydrocele does not spontaneously resolve, or if symptoms are significant, a surgical procedure known as a hydrocelectomy may be recommended. The key aspects of hydrocelectomy include:
Preparation for Surgery
- The procedure is often performed as an outpatient surgery, meaning hospitalization overnight is not usually required.
- Anesthesia is administered prior to surgery; this may be general anesthesia (causing sleep-like state) or spinal anesthesia (numbing the lower part of the body).
- Preoperative instructions may include fasting, discontinuation of certain medications, and arranging for transportation after the procedure.
Surgical Procedure
- The surgeon makes an incision in the scrotum or lower abdomen, depending on the location and size of the hydrocele.
- Fluid is drained, and the hydrocele sac may be removed or repaired.
- Occasionally, a hydrocele is discovered and removed during surgery intended for other reasons, such as inguinal hernia repair.
- Surgical closure is performed, and sterile dressings are placed over the incision site.
Table: Key Steps of Hydrocelectomy
| Step | Description |
|---|---|
| Anesthesia | General or regional (spinal) anesthesia to ensure comfort and pain control. |
| Incision | Scrotal or abdominal incision to access the hydrocele sac. |
| Drainage / Removal | Fluid is drained; the hydrocele sac is excised or corrected. |
| Closure | Incision is closed; dressing applied. |
Postoperative Care
- Patients may need to wear a bulky bandage for a few days and may have a tube in place to help drain residual fluid.
- Pain and swelling are common after surgery and can be managed with pain relievers, scrotal support, and ice packs.
- Heavy lifting, vigorous exercise, and sexual activity should be avoided for a period specified by the healthcare provider, usually several weeks.
- A follow-up appointment is necessary to monitor healing and manage any complications or hydrocele recurrence.
Risks and Potential Complications
- Surgical risks include infection, bleeding, hematoma (collection of blood), scrotal bruising, and injury to surrounding structures.
- Recurrent hydrocele formation can occur, necessitating further intervention.
- Risks are generally low, and hydrocelectomy is considered a safe procedure with a high success rate.
Alternative and Supportive Care Measures
Currently, there are no medications or non-surgical methods proven to definitively reduce or eliminate hydroceles. The standard supportive measures include:
- Observation for spontaneous resolution, especially in infants and non-painful adult cases.
- Scrotal support garments may provide temporary relief from discomfort.
- Application of cold compresses or ice packs may help minimize swelling after intervention.
When to Seek Medical Attention
Prompt evaluation by a healthcare provider is necessary if:
- Scrotal swelling is sudden, painful, or associated with redness or warmth.
- The hydrocele increases rapidly in size.
- Other symptoms develop, such as fever or persistent discomfort.
These signs may indicate underlying infection, hernia, testicular torsion, or other serious conditions requiring urgent attention.
Recovery and Outlook After Treatment
Most people recover well after hydrocele surgery. Key recovery aspects include:
- Pain and swelling typically decrease over several days to a few weeks post-surgery.
- Normal activities may be resumed within several days, but full recovery can take a few weeks.
- Long-term outlook is excellent, with most patients experiencing complete symptom relief and minimal recurrence risk.
Departments and Specialties Involved in Hydrocele Care
Expert care for hydrocele is commonly provided by:
- Pediatric Surgery (for children and infants)
- Urology (for adults and surgical management)
- General surgery and family medicine may also be involved in diagnosis and symptom management.
Frequently Asked Questions (FAQs)
Q: What causes a hydrocele?
A: Hydroceles may develop due to incomplete closure of a membrane during fetal development, or secondary to trauma, infection, inflammation, or surgery in older children and adults.
Q: Are hydroceles dangerous?
A: Most hydroceles are benign and do not pose serious health risks. However, evaluation is important to rule out other underlying issues.
Q: When is surgery necessary for a hydrocele?
A: Surgery is recommended if a hydrocele causes pain, is very large, interferes with daily life, or does not resolve spontaneously.
Q: Can a hydrocele recur after surgery?
A: While rare, recurrence can occur, particularly if underlying causes are not addressed. Regular follow-up can help manage or prevent recurrence.
Q: How long is the recovery after hydrocelectomy?
A: Most people return to normal activities within a few days, but full recovery can take a few weeks. Individual recovery times may vary.
Q: Does a hydrocele increase the risk of infertility?
A: Hydroceles are usually not associated with impaired fertility. However, if they coexist with other testicular conditions, additional evaluation is recommended.
Key Takeaways
- Hydroceles are fluid accumulations in the scrotum and are usually harmless.
- Diagnosis relies on physical exam, transillumination, and sometimes ultrasound.
- Observation is recommended in many cases, but persistent or bothersome hydroceles may require surgery.
- Hydrocelectomy is safe, effective, and generally leads to excellent long-term outcomes.
- Prompt medical assessment helps exclude more serious conditions and guides appropriate care.
References
- https://www.mayoclinic.org/diseases-conditions/hydrocele/diagnosis-treatment/drc-20363971
- https://my.clevelandclinic.org/health/diseases/16294-hydrocele
- https://lincolntonfamilydoctors.com/wp-content/uploads/2017/11/Hydrocele.pdf
- https://www.mayoclinic.org/diseases-conditions/hydrocele/doctors-departments/ddc-20364953
- https://my.clevelandclinic.org/health/procedures/16232-hydrocelectomy
- https://www.mayoclinic.org/diseases-conditions/varicocele/diagnosis-treatment/drc-20378772
- https://www.mayoclinic.org/diseases-conditions/hydrocele/symptoms-causes/syc-20363969
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/hydrocele
- https://monument.health/mayo-clinic-health-information-library/article/?mayo-id=ABT-20329551
- https://www.amerikanhastanesi.org/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/hydrocele
Read full bio of medha deb