Meningitis: Symptoms, Causes, and When to Seek Help
Learn about the causes, symptoms, risk factors, and treatments for meningitis—a serious infection of the brain and spinal cord membranes.
Overview
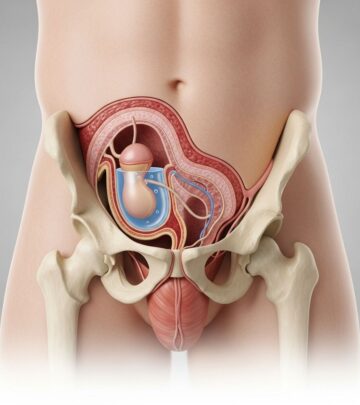
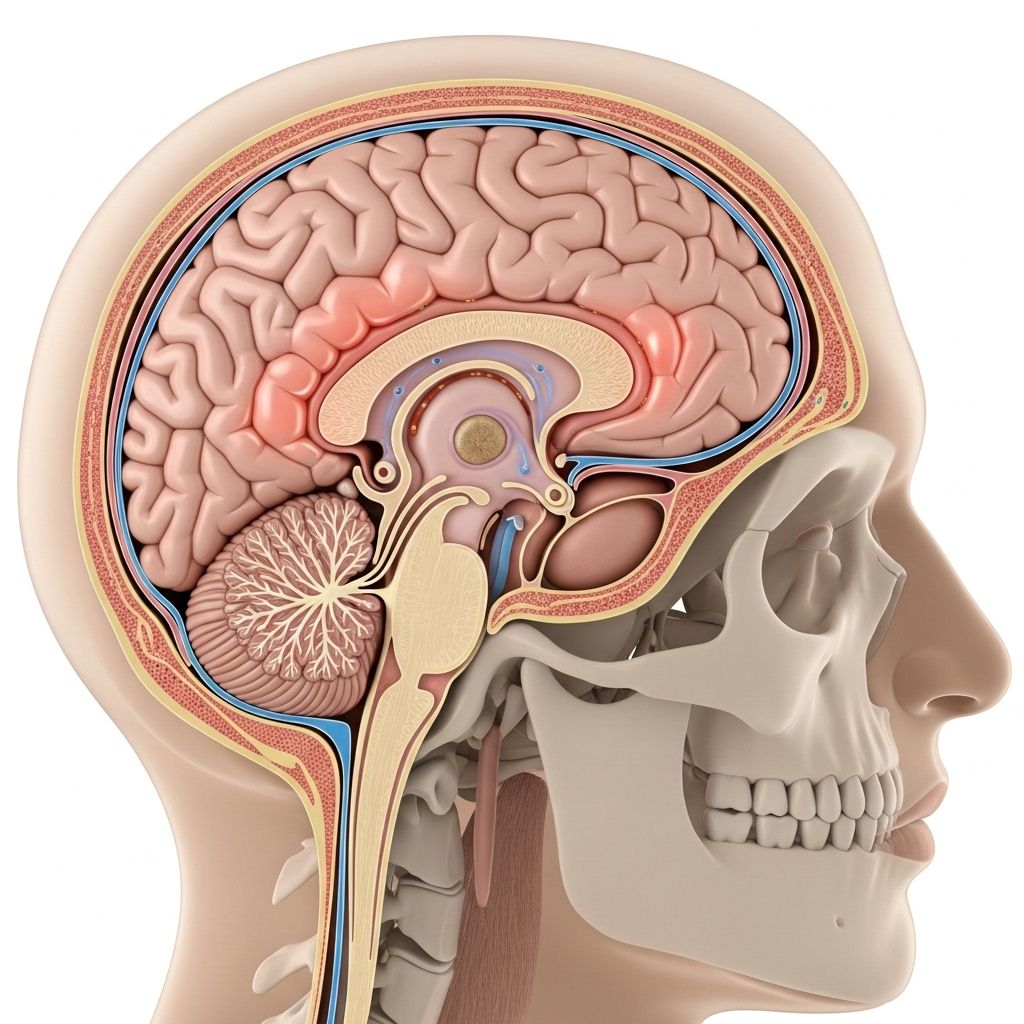
Meningitis is an inflammation of the membranes (meninges) surrounding your brain and spinal cord. This swelling is most often caused by an infection, though it can also result from noninfectious causes. The infection can be bacterial, viral, fungal, or even parasitic. Some cases of meningitis improve on their own, while others are life-threatening and require immediate medical attention.
Symptoms
Meningitis symptoms can develop suddenly and may overlap with those of the flu, making initial diagnosis challenging. Common symptoms in people older than 2 years include:
- Sudden high fever
- Severe headache
- Stiff neck
- Nausea or vomiting
- Confusion or difficulty concentrating
- Seizures
- Sleepiness or trouble waking up
- Sensitivity to light
- Skin rash (sometimes, such as in meningococcal meningitis)
In newborns and infants, symptoms may include:
- High fever
- Constant crying
- Excessive sleepiness or irritability
- Poor feeding
- Bulge in the soft spot on the head (fontanel)
- Stiffness in the body and neck
If you or someone you know has symptoms of meningitis—especially a severe headache, high fever, stiff neck, confusion, or vomiting—seek medical care immediately. Delayed treatment for bacterial meningitis increases the risk of serious complications, including permanent brain damage or death.
Causes
Meningitis can result from a variety of causes, which generally fall into infectious and noninfectious categories.
Infectious Causes
- Viral meningitis: The most common form in the United States, usually mild and often clears on its own. Most cases are caused by enteroviruses, which are most prevalent in late summer and early fall. Other viruses that can cause meningitis include herpes simplex virus, HIV, mumps, and West Nile virus.
- Bacterial meningitis: Less common but much more serious, potentially fatal within days without prompt treatment. The bacteria can enter the bloodstream and travel to the brain or directly invade the meninges. The most common causes are Neisseria meningitidis (meningococcal meningitis, highly contagious, often affecting teenagers and young adults), Streptococcus pneumoniae, and Haemophilus influenzae. Bacterial meningitis is a medical emergency.
- Fungal and parasitic meningitis: These forms are rare but can be serious, especially in people with weakened immune systems. Cryptococcal meningitis, for example, is a common fungal form associated with AIDS.
Noninfectious Causes
Meningitis can also be triggered by noninfectious causes, such as:
- Chemical reactions
- Drug allergies
- Certain cancers
- Inflammatory diseases such as sarcoidosis
Risk Factors
Several factors can increase the risk of developing meningitis:
- Age: Young children, adolescents, and young adults (college students living in dormitories, military recruits) are at higher risk for bacterial meningitis.
- Community settings: Living in close quarters (such as college dorms, military barracks) can facilitate the spread of meningococcal disease.
- Medical conditions: Weakened immune system (from HIV/AIDS, diabetes, immunosuppressive therapy), missing spleen, or chronic illness.
- Travel: Certain regions have higher rates of bacterial or parasitic meningitis.
- Pregnancy: Pregnant women are at increased risk of listeriosis, which can lead to meningitis.
Complications
Meningitis can lead to serious complications, especially if not treated promptly:
- Hearing loss
- Memory difficulties
- Learning disabilities
- Brain damage
- Gait or movement problems
- Seizures
- Kidney failure
- Shock
- Death
Prevention
Vaccination is the most effective way to prevent some types of bacterial meningitis:
- Meningococcal vaccines: The CDC recommends routine vaccination for all 11- to 12-year-olds with a booster at age 16. College students, military recruits, and others at high risk may need additional doses.
- Pneumococcal vaccines: Protect against infections caused by Streptococcus pneumoniae.
- Hib vaccine: Protects against Haemophilus influenzae type b (Hib).
Other preventive measures include:
- Practicing good hygiene (regular handwashing, not sharing personal items)
- Staying healthy (getting enough sleep, exercising, eating a balanced diet)
- Avoiding close contact with people who are sick
Diagnosis
Diagnosing meningitis typically involves:
- Medical history and physical exam: Checking for typical signs such as fever, stiff neck, and altered mental status.
- Lumbar puncture (spinal tap): Collecting cerebrospinal fluid for analysis to determine the cause of meningitis.
- Blood tests: To identify infection, inflammation, and antibodies.
- Imaging tests: CT or MRI scans to detect complications such as swelling or abscess.
Prompt diagnosis and treatment are crucial to prevent severe complications, especially in bacterial meningitis.
Treatment
Treatment depends on the cause of meningitis:
- Bacterial meningitis: Requires immediate hospital care and intravenous antibiotics. Corticosteroids may be given to reduce inflammation. Close contacts may also receive preventive antibiotics.
- Viral meningitis: Usually resolves on its own. Supportive care includes rest, fluids, and pain relief medications. Antiviral medications may be used if caused by herpes viruses.
- Fungal meningitis: Treated with antifungal medications, often for prolonged periods.
- Noninfectious meningitis: Management depends on the underlying cause (e.g., avoiding offending drugs, treating an autoimmune condition).
Preparing for Your Appointment
If you suspect meningitis or are being evaluated for it, prepare for your appointment by:
- Writing down symptoms, including when they started
- Noting any recent exposures to illnesses or travel history
- Listing medications, vitamins, and supplements you take
- Bringing a family member or friend to help remember information
Be prepared to answer questions about symptoms, medical history, and potential exposures to infection.
When to See a Doctor
Seek immediate medical attention if you or someone else has:
- Fever, severe headache, and a stiff neck
- Confusion or seizures
- Vomiting
- Skin rash that looks like bruises or small reddish or purple spots
Bacterial meningitis requires emergency treatment. Also, talk to your doctor if you have been in close contact with someone diagnosed with meningitis, as you may need preventive medication.
Frequently Asked Questions (FAQs)
Q: How is meningitis spread?
Viral and bacterial meningitis can be spread through respiratory secretions (coughing, sneezing) or close contact with an infected person. Some types, like fungal or noninfectious meningitis, are not contagious.
Q: Is there a vaccine for meningitis?
Yes, vaccines are available for some types of bacterial meningitis, including meningococcal, pneumococcal, and Hib vaccines. They are recommended for children, adolescents, and those at increased risk.
Q: Can I get meningitis more than once?
Yes, it is possible to develop meningitis again, especially from a different organism or cause. Recurrence is rare but can occur.
Q: How long does it take to recover from meningitis?
Recovery depends on the cause and severity. Viral meningitis usually resolves in a few weeks. Bacterial meningitis recovery may take longer, and some people experience long-term complications.
Q: Is meningitis contagious?
Viral and bacterial meningitis can be contagious, especially among close contacts. Fungal and noninfectious meningitis are not contagious.
Summary Table: Types of Meningitis
| Type | Causes | Severity | Contagious | Preventable |
|---|---|---|---|---|
| Bacterial | Bacteria (e.g., N. meningitidis, S. pneumoniae, H. influenzae) | Severe, can be fatal | Yes | Yes (vaccines available) |
| Viral | Viruses (e.g., enteroviruses, herpes simplex, mumps) | Usually mild | Yes | No |
| Fungal | Fungi (e.g., Cryptococcus) | Severe in immunocompromised | No | No |
| Parasitic | Parasites (rare) | Variable | No | No |
| Noninfectious | Chemical reaction, cancer, autoimmune disease | Variable | No | No |
Conclusion
Meningitis is a serious condition that requires prompt recognition and treatment. While some forms are mild, others—especially bacterial meningitis—can be life-threatening. Understanding the symptoms, risk factors, and prevention strategies is crucial for protecting yourself and your community. Vaccination remains the most effective way to prevent certain types of bacterial meningitis, and immediate medical attention is essential if you suspect meningitis.
Read full bio of medha deb