Miscarriage: Causes, Symptoms, and Risk Factors Explained
Learn about miscarriage: symptoms, causes, risk factors, and what to expect for recovery and support.

Miscarriage—the unexpected loss of a pregnancy before the 20th week—is a challenging and often unexpected event. While miscarriage is common, affecting about 10% to 20% of known pregnancies, the actual rate is likely higher due to very early losses that may occur before a pregnancy is recognized. This article examines in detail the causes, symptoms, risk factors, and what people experiencing pregnancy loss should know about diagnosis, support, and recovery.
Overview
A miscarriage is a sudden pregnancy loss that occurs before 20 weeks gestation. Most miscarriages happen in the first trimester, within the first 13 weeks. The term itself can be misleading, as it may suggest the pregnant person did something wrong. In reality, the vast majority of miscarriages happen because the embryo or fetus does not develop properly—in most cases due to factors beyond anyone’s control.
- Miscarriage occurs in 10%–20% of recognized pregnancies.
- The true rate is likely higher due to very early losses.
- Most miscarriages result from issues with fetal development, especially genetic problems.
Understanding what causes miscarriage, which symptoms to watch for, and what risk factors may be involved can help move toward emotional and physical healing after such loss.
Symptoms
Most miscarriages take place in the first trimester (the first 13 weeks of pregnancy). However, symptoms may occur at any time before 20 weeks. Recognizing the signs of miscarriage is important to seek timely medical attention.
- Bleeding from the vagina: This may be light spotting or heavier bleeding, sometimes with clots.
- Pelvic pain or cramping: Pain can occur in the abdomen or lower back.
- Passing fluid or tissue from the vagina: Sometimes tissue from the pregnancy may be expelled.
- Rapid heartbeat (tachycardia): Occasionally occurs during or after miscarriage.
Important: Not all vaginal bleeding in early pregnancy ends in miscarriage. Many pregnancies with early bleeding continue successfully. However, if bleeding is heavy or accompanied by pain or tissue passage, seek immediate medical advice.
If any tissue is passed, collect it in a clean container and bring it to your healthcare provider, who may send it for analysis. This can help determine if a miscarriage has occurred and, occasionally, the underlying cause.
Causes
The causes of miscarriage are varied, with most rooted in problems with the genetic material of the embryo or fetus.
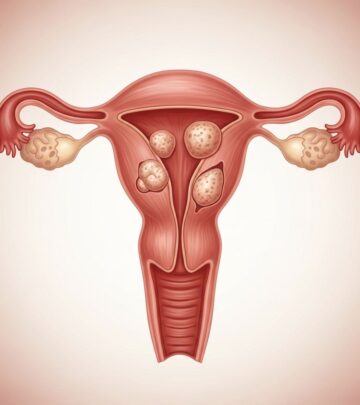
Irregular Genes or Chromosomes
About half to two-thirds of miscarriages in the first trimester are linked to chromosomal abnormalities, meaning the embryo or fetus has too many or too few chromosomes. Chromosomes are packages of genes that instruct the body’s development. Problems arise most often by chance as the embryo forms, not due to anything the parents did.
- Anembryonic pregnancy (blighted ovum): No embryo develops, or the embryo stops developing very early and is absorbed by the body.
- Intrauterine fetal demise: The embryo forms but then stops developing and dies, often with no immediate symptoms.
- Molar or partial molar pregnancy: These rare conditions result from abnormal fertilization and chromosomal content, leading to growths in the placenta rather than normal fetal development.
| Type of Chromosomal Problem | Description / Outcome |
|---|---|
| Anembryonic pregnancy (Blighted Ovum) | No embryo forms, only a gestational sac is seen. Always results in miscarriage early in pregnancy. |
| Intrauterine fetal demise | Embryo starts forming but stops developing and dies before pregnancy loss symptoms appear. |
| Molar pregnancy | Abnormal tissue grows in the uterus, often due to two sets of chromosomes coming from the sperm. Embryo does not develop properly. |
| Partial molar pregnancy | Some fetal tissue may develop along with abnormal placental tissue. Not viable and may cause health problems. |
Molar and partial molar pregnancies can cause serious complications for the pregnant person. Sometimes, changes in the placenta may even lead to the development of rare pregnancy-related cancers, so these situations require specific management and follow-up.
Other Causes of Miscarriage
- Maternal health conditions: While not as common as genetic causes, certain maternal illnesses increase miscarriage risk. Examples include poorly controlled diabetes, thyroid disease, or uterine abnormalities.
- Infections: Severe infection—either related to the pregnancy or affecting maternal health—can occasionally result in miscarriage.
- Lifestyle factors: Smoking, heavy alcohol use, illicit drug use, and excessive caffeine intake have all been associated with increased risk of miscarriage.
- Age: The risk of miscarriage increases with maternal age, especially after 35.
- Environmental factors: Severe exposure to environmental toxins, radiation, or traumatic injury may, rarely, lead to miscarriage.
Risk Factors
Certain factors make miscarriage more likely, although the direct cause is often unknown.
- Maternal Age: After age 35, risk rises; after 40, the risk increases even more appreciably.
- History of Previous Miscarriages: Having two or more consecutive miscarriages raises the risk of another miscarriage.
- Chronic medical conditions: Such as uncontrolled diabetes or thyroid problems.
- Uterine or cervical problems: Physical abnormalities may also contribute.
- Infections: Including certain viral or bacterial infections.
- Lifestyle habits: Smoking, alcohol, illicit drugs, and excess caffeine intake.
- Weight: Underweight or obesity may affect miscarriage risk.
Myths and Misconceptions
Many people experiencing miscarriage wonder if something they did caused the loss. Research confirms that ordinary activities—such as exercise, working, having sexual intercourse, or minor injuries—do not cause miscarriage. Emotional stress also does not directly cause early pregnancy loss. Most often, miscarriage is due to random chromosomal errors, entirely outside anyone’s control.
Diagnosis
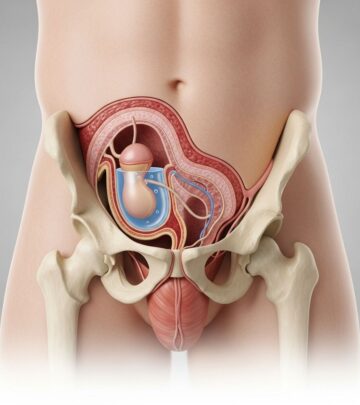
If symptoms of miscarriage occur, or a healthcare provider suspects pregnancy loss during a routine checkup, several methods help confirm the diagnosis:
- Ultrasound: The standard and most accurate test. It checks for fetal heartbeat and appropriate development for gestational age.
- Blood tests: Measure levels of human chorionic gonadotropin (hCG)—a hormone made during pregnancy. Declining or low hCG may indicate loss.
- Pelvic exam: Checks for cervical dilation, bleeding, or passage of tissue.
- Analysis of passed tissue: If tissue is expelled, it may be sent to a lab to confirm pregnancy loss and help identify the cause.
Treatment and What to Expect
The course of treatment depends on the type and timing of miscarriage and the physical health of the person affected.
- Expectant management: Allowing the miscarriage to progress naturally if no infection or complications are present. The body typically expels all pregnancy tissue over time.
- Medication: If tissue doesn’t pass on its own, medication can help complete the miscarriage safely.
- Surgical procedures: If tissue remains or complications develop, a procedure known as dilation and curettage (D&C) may be needed to remove remaining pregnancy tissue from the uterus.
After a miscarriage, a follow-up visit ensures that the uterus is empty and no infection or other complication has occurred.
Emotional Impact and Recovery
Experiencing a miscarriage brings not only physical but also profound emotional effects. Feelings of grief, guilt, anger, and sadness are normal responses. Support from family, friends, healthcare teams, or professional counseling can help the healing process.
- Support groups: Joining a pregnancy loss support group may assist in navigating loss and sharing experiences with others.
- Counseling: Professional counseling or therapy is recommended for those with ongoing depression, anxiety, or trauma after miscarriage.
Frequently Asked Questions (FAQs)
Q: What is the most common cause of a miscarriage?
A: The leading cause is genetic or chromosomal abnormalities that occur randomly as the embryo forms. This is not caused by anything the parents did or did not do.
Q: Can exercise, working, or stress cause miscarriage?
A: No. Ordinary activities, including moderate exercise and working, do not cause miscarriage. Early miscarriage is not caused by emotional stress.
Q: Do most people who have had a miscarriage go on to have successful pregnancies?
A: Yes. Most people who experience a single miscarriage have healthy future pregnancies. However, several consecutive losses may warrant further evaluation.
Q: When should I contact my healthcare provider during pregnancy?
A: Seek prompt evaluation for any heavy vaginal bleeding, severe cramping, passing tissue, or other concerning symptoms during the first 20 weeks of pregnancy.
Q: What support is available for those coping with miscarriage?
A: Support groups, mental health professionals, and counseling services are all helpful resources for navigating the emotional aftermath of pregnancy loss.
Preventing Miscarriage: Is It Possible?
It’s not possible to prevent most miscarriages, especially those caused by random chromosomal errors. However, certain steps may promote a healthy pregnancy:
- Seek regular prenatal care as soon as pregnancy is confirmed.
- Manage existing health conditions, such as diabetes or thyroid problems.
- Avoid smoking, alcohol, and illicit drugs.
- Limit caffeine to less than 200 mg per day (about one 12-oz cup of coffee).
- Maintain a healthy weight before and during pregnancy.
If you’ve experienced more than two miscarriages in a row, consider genetic counseling or specialized evaluation to rule out underlying factors.
Key Takeaways
- Miscarriage is a common occurrence, with most cases happening in the first 13 weeks.
- Chromosomal abnormalities are by far the most frequent cause, and most are unavoidable.
- Symptoms include vaginal bleeding, pain, and sometimes passage of tissue.
- Consult a healthcare provider for diagnosis and guidance as soon as symptoms appear.
- Emotional support and self-compassion are critical components of healing after pregnancy loss.
By understanding miscarriage with accurate, compassionate information, those affected can take important steps toward both physical recovery and emotional well-being.
References
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/definitions/miscarriage
- https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes/syc-20354298
- https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/miscarriage
- https://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy-after-miscarriage/art-20044134
- https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/diagnosis-treatment/drc-20354304
- https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/early-miscarriage/faq-20058214
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/miscarriage-its-not-your-fault
- https://my.clevelandclinic.org/health/diseases/9688-miscarriage
Read full bio of Sneha Tete