Peyronie’s Disease: Diagnosis and Comprehensive Treatment Options
Explore diagnosis and tailored treatment solutions for Peyronie’s disease, from early interventions to advanced therapies for optimal men’s health.
Peyronie’s Disease: Diagnosis and Treatment
Peyronie’s disease is a frequently misunderstood condition that can have a substantial impact on men’s physical health, psychological well-being, and intimate relationships. Characterized primarily by fibrous scar tissue development in the penis, Peyronie’s disease can result in penile curvature, pain, shortening, and erectile dysfunction. This article explores diagnostic pathways and the full range of individualized, evidence-based treatments offered by leading centers, such as Mayo Clinic, ensuring patients receive comprehensive, patient-centered care.
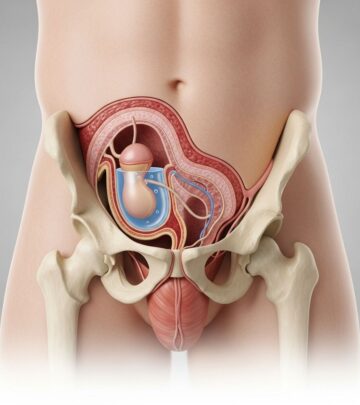
Understanding Peyronie’s Disease
Peyronie’s disease involves the formation of fibrous scar tissue (plaque) along the tunica albuginea, the sheath surrounding erectile tissue in the penis. This disrupts the uniform expansion during erection, provoking painful, bent, or sometimes indented erections. The severity of these effects can vary widely among individuals, influencing when and how treatment is considered.
- Men of all ages may develop Peyronie’s disease; cases range from teenage years to patients in their 70s and beyond.
- Not all patients recall an episode of trauma; microtrauma (minor injury, often cumulative) is thought to be a trigger, especially in men with genetic susceptibility.
- Peyronie’s disease is benign, but symptoms can significantly affect sexual function and quality of life.
Diagnosis of Peyronie’s Disease
The diagnostic process for Peyronie’s disease typically focuses on clinical evaluation, patient history, and direct examination of penile deformity. Definitive diagnosis allows clinicians to tailor treatment to disease severity and patient priorities.
Key Steps in Diagnosis
- Medical history: Assessment of symptom onset, progression, erectile function, pain, and prior trauma.
- Physical exam: Palpation of penile shaft to identify plaques; assessment during erection when possible.
- Imaging (optional): Ultrasound can characterize plaque and rule out calcification.
- Measurement of curvature: Artificial erection may be induced in-house to measure curve and other deformities with a goniometer, offering more precise evaluation than photos alone.
A formal assessment in the erect state is recommended when symptoms are severe enough to consider intervention.
Treatment Approaches by Disease Stage
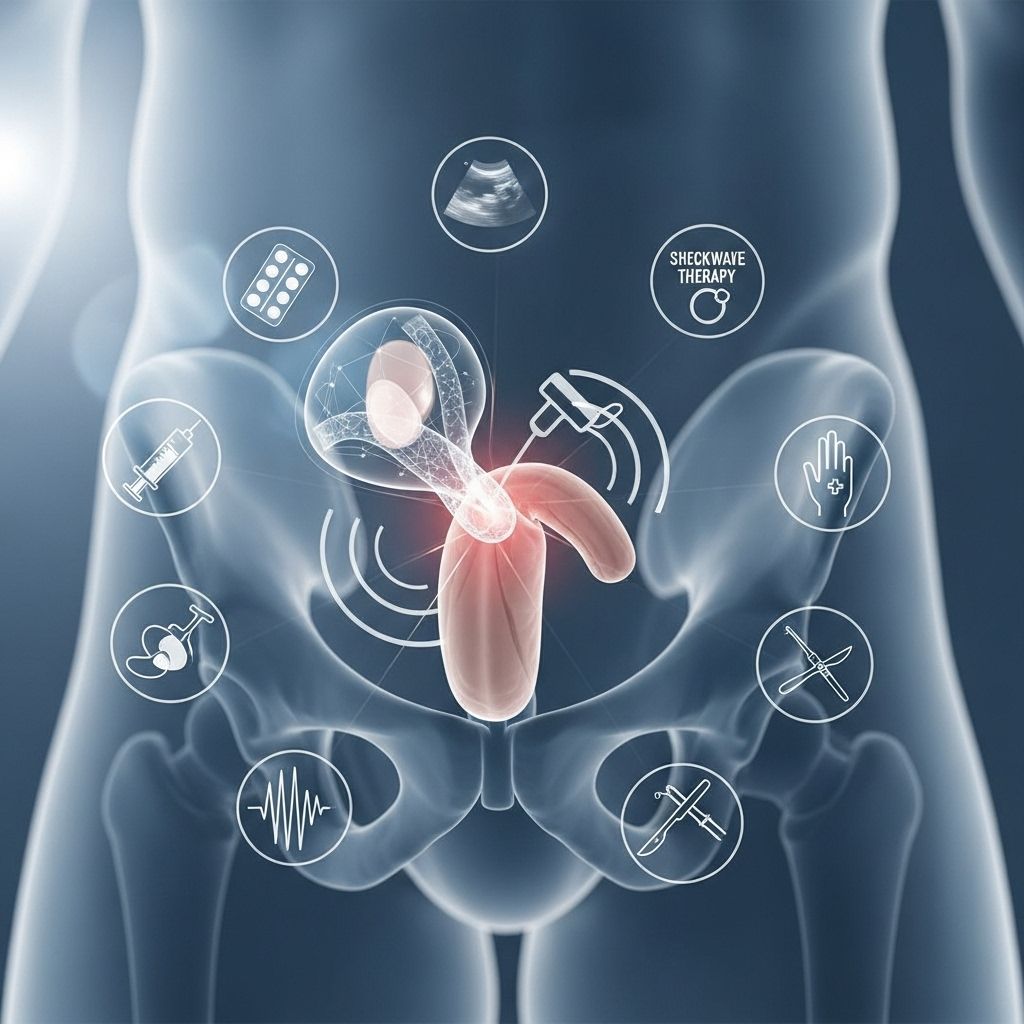
Effective treatment of Peyronie’s disease depends on the stage of the condition and the impact on the patient’s life. Therapy is highly individualized—ranging from observation and counseling to medical, non-surgical and surgical interventions.
Defining Disease Stages
- Acute phase: Lasts 5–18 months. Scar tissue is still forming, and changes in curvature or length may continue. Erectile pain is often present.
- Chronic phase: Scar formation stabilizes. Curvature, deformity, and penile pain typically stop progressing or resolve, making intervention more predictable and safer.
Acute Phase Peyronie’s Disease: Management Strategies
During the acute phase, the focus is on preventing further deformity and managing pain, as the disease’s natural evolution makes surgical correction inappropriate at this time.
Available Treatments
- Penile Traction Therapy
- Utilizes a device that holds the penis in a cradle and applies gentle, consistent tension.
- Early use may help prevent length loss and minimize curvature progression.
- Demonstrated to increase penile length in select patients when used consistently over months.
- Medications
- Both oral and injectable therapies have been tested for Peyronie’s disease; evidence of efficacy varies.
- Certain oral agents commonly used in the past (such as vitamin E, potassium para-aminobenzoate) do not have proven benefit.
- Collagenase clostridium histolyticum (XIAFLEX), a prescription injection, is the only FDA-approved medication for treating penile curvature (see below).
- Counseling and Education
- Reassurance that the disease is non-cancerous and non-life-threatening.
- Support for managing psychological effects while waiting for disease stabilization.
Surgery is generally avoided, as outcomes are unpredictable until deformity ceases progressing and pain resolves. Surgery during this time may necessitate additional corrections in the future.
Chronic Phase Peyronie’s Disease: Individualized Treatment Options
Once Peyronie’s disease has stabilized (chronic phase), and pain is absent or minimal, more definitive treatment options are considered for patients who are significantly bothered by their symptoms.
Medical and Non-surgical Therapies
- Collagenase Injections (XIAFLEX): The only FDA-approved, minimally invasive therapy shown to improve curvature and some symptoms in eligible patients with stable plaques and measurable curve. Several cycles of treatment are often necessary.
- Penile Traction Devices: Can be continued for stable cases to maintain or improve length and curvature, especially when used alongside other therapies.
- Oral Medications: Typically, oral medications alone are not effective for established Peyronie’s disease in the chronic phase.
Surgical Solutions
Surgery is the gold standard for men with severe curvature, deformity, or erectile dysfunction that impairs sexual function, especially when conservative management has failed or is inappropriate.
| Procedure | Who is it for? | Key Details |
|---|---|---|
| Penile Plication | Men with good erectile function and less severe curvature | Sutures placed to straighten the penis; minimal effect on length |
| Plaque Incision/Excision and Grafting | Men with severe curves, complex deformities, or indentation | Plaque is cut (incised) or removed (excised), and a graft covers the gap. May impact erectile firmness. |
| Penile Prosthesis Implantation | Men with significant erectile dysfunction, sometimes with ED and Peyronie’s disease together | Inflatable or malleable prosthesis placed. Often straightens curvature and restores rigidity. |
- Choice of surgical method depends on: curvature severity, penile length, erectile function, and patient preferences.
- Procedures are very successful, but each carries unique risks and benefits. A thorough discussion of expectations and possible side effects is routine.
Psychological and Relationship Support
Peyronie’s disease can be distressing. Counseling from experienced providers, and in some cases, mental health support, are important components of comprehensive care, addressing the psychological and relationship impacts of the condition.
Comparison of Non-Surgical and Surgical Treatments
| Non-Surgical Treatments | Surgical Treatments |
|---|---|
|
|
| Best for mild to moderate symptoms, or when curvature/stability allow | Best for severe curvature, complex deformity, or significant erectile dysfunction |
| Noninvasive or minimally invasive; lower risk profile | Invasive; higher but manageable risk profile |
The Mayo Clinic Approach to Peyronie’s Disease
Mayo Clinic specialists emphasize an individualized, evidence-based approach to diagnosis and treatment:
- A thorough evaluation by experienced urologists familiar with the latest evidence and guidelines.
- Emphasis on shared decision-making to tailor therapy based on patient concerns, disease phase, and overall health.
- Comprehensive experience in all non-surgical therapies, injectable treatments (including high volume practice in collagenase administration), and complex surgical solutions.
- Understanding and addressing the psychological impacts through expert counseling and, when needed, mental health support.
- Elimination of myths and misinformation through patient education, fostering realistic expectations and informed choices.
Frequently Asked Questions (FAQs)
What is Peyronie’s disease?
Peyronie’s disease is a connective tissue disorder where scar tissue develops within the penis, leading to curvature, pain, and sometimes erectile dysfunction, especially during erections.
Who is at risk for Peyronie’s disease?
Any man may develop Peyronie’s disease, though it tends to affect men between 40 and 70. It can occur in younger or older men as well.
Is Peyronie’s disease dangerous or cancerous?
No, it is a benign (non-cancerous) condition, but it can have a significant impact on sexual function and mental health.
When should someone seek treatment?
Men bothered by pain, visible curvature, difficulties with intercourse, or distress related to penile changes should seek evaluation. Not all cases require intervention.
Can Peyronie’s disease get better on its own?
Up to 13% of cases may experience some improvement without intervention, but most stabilize with persistent curvature unless actively treated.
Are oral medications helpful for Peyronie’s disease?
Most oral medications, including vitamin E and potassium para-aminobenzoate, have not shown clear benefit in clinical studies and are not routinely recommended.
Is surgery always necessary?
No. Surgery is reserved for those with severe, stable curvature or erectile dysfunction that impairs sexual function, and who have not responded to non-surgical treatments.
Key Points and Takeaway Messages
- Peyronie’s disease is more common than often recognized and can affect men of all ages.
- Diagnosis involves medical history, physical examination, and possibly imaging or in-clinic measurement.
- Treatment should be individualized, focusing on the phase of disease, severity of symptoms, and patient preferences.
- Non-surgical and surgical therapies can provide meaningful improvement, especially when managed by experienced teams using evidence-based protocols.
- Psychological support is a vital element of comprehensive care for those affected by Peyronie’s disease.
Additional Resources
- Consult a board-certified urologist or men’s health specialist for an accurate diagnosis and personal treatment plan.
- Access clinical trials for new therapies (when suitable and available).
- Seek psychological support or counseling to address the mental health impact of the condition.
Read full bio of Sneha Tete