Pseudomembranous Colitis: Symptoms, Causes, and Risk Factors
Explore the symptoms, causes, and risk factors of pseudomembranous colitis, an inflammatory colon condition linked with C. difficile infection.
Pseudomembranous Colitis
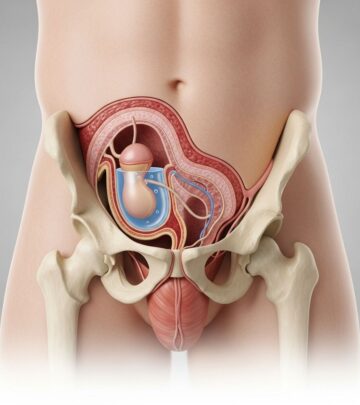
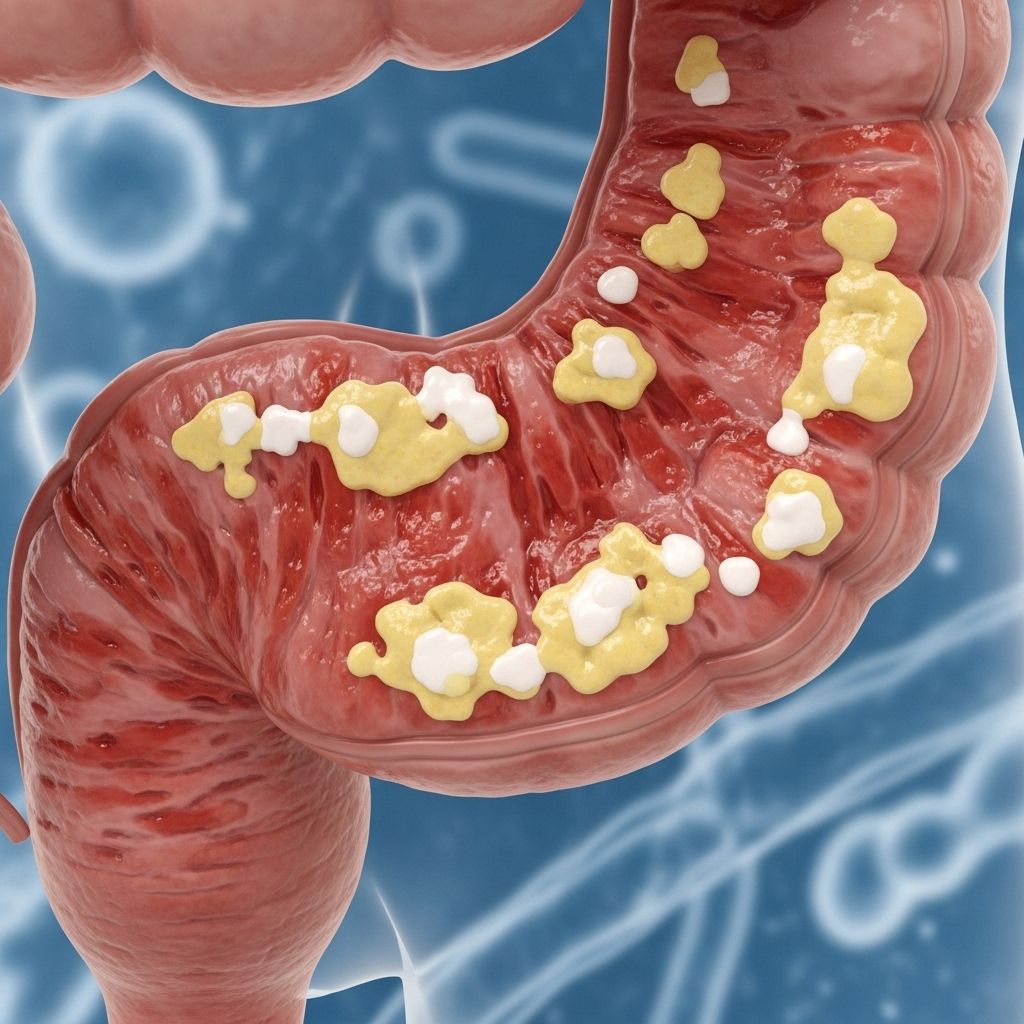
Pseudomembranous colitis is an acute inflammation of the colon (large intestine) most commonly associated with an overgrowth of the bacterium Clostridioides difficile, also known as C. difficile or C. diff. This condition, sometimes referred to as antibiotic-associated colitis or C. difficile colitis, is characterized by the formation of yellow-white plaques, called pseudomembranes, on the colon wall, resulting from cellular injury and immune response.
Overview
Pseudomembranous colitis typically arises following disruption of the normal gut bacterial balance, most often due to the use of antibiotics. When C. difficile outgrows other bacteria, it releases toxins—chiefly toxin A and toxin B—that can severely damage the colon’s lining, causing symptoms from watery diarrhea to fever and abdominal pain.
Symptoms
The primary symptoms of pseudomembranous colitis include:
- Watery diarrhea (may begin as soon as 1–2 days after starting antibiotics or weeks to months after finishing them)
- Stomach cramps, tenderness, or pain
- Fever
- Pus or mucus in stool
- Nausea
- Dehydration
- Blood in stool (less common)
Symptoms can vary in severity. Mild cases may only include diarrhea and mild abdominal discomfort, while severe forms may produce 10–15 episodes of diarrhea per day, significant blood loss, dehydration, and a swollen belly.
| Symptom | Description |
|---|---|
| Watery diarrhea | Frequent, liquid bowel movements. |
| Stomach pain/cramping | Discomfort, pain or tenderness in abdomen. |
| Fever | Elevated body temperature (often above 38°C). |
| Pus or mucus in stool | Visible white or yellowish substance in feces. |
| Nausea | Feeling the urge to vomit. |
| Dehydration | Signs include dry mouth, lethargy, and dizziness. |
| Blood in stool | Red or dark streaks; less common. |
When to Seek Medical Attention
If you are currently taking or have recently taken antibiotics and experience diarrhea, contact your healthcare provider—even if symptoms seem mild. Also, seek medical care if you develop severe diarrhea accompanied by fever, painful stomach cramps, or blood/pus in stool.
Causes
The chief cause of pseudomembranous colitis is infection by C. difficile. Normally, a healthy colon maintains a balance of many bacterial species. However, when antibiotics or other medications disrupt this balance, C. difficile can quickly proliferate:
- Antibiotics diminish competing bacteria, allowing C. difficile overgrowth.
- C. difficile produces toxins that damage colon lining, causing cell death and inflammation.
- Pseudomembranes form from cellular debris and white blood cells gathering at the injury site.
While C. difficile infection (CDI) is responsible for over 90% of pseudomembranous colitis cases, other types of colon injury—including other bacterial, viral, or parasitic infections—can also cause similar damage, though much less commonly.
Antibiotics Most Commonly Associated
- Ampicillin
- Clindamycin
- Cephalosporins
- Fluoroquinolones
Almost any antibiotic can contribute, but these classes bear the highest risk.
Other Medications and Causes
- Chemotherapy drugs (used for cancer) that disturb bacterial balance
- Immunosuppressive medicines that weaken the immune system
- Surgical procedures involving the colon
Additionally, diseases that affect the colon—such as ulcerative colitis, Crohn’s disease, or inflammatory bowel disease (IBD)—may increase vulnerability, sometimes even without antibiotic use.
Transmission and Spread
C. difficile spores are highly resistant to common disinfectants and can persist on surfaces for extended periods. Transmission is most common:
- In healthcare settings, from the hands of medical professionals or contaminated surfaces
- Among people with recent hospital stays or surgery
- Through contact with contaminated objects in communal environments
Increasingly, C. difficile infections are recognized in people without classic risk factors, including those with no recent healthcare contact or antibiotic exposure. This form is termed community-acquired C. difficile.
Risk Factors
Certain factors amplify the risk of developing pseudomembranous colitis:
- Older age (particularly over 65)
- Antibiotic use
- Recent hospitalization or surgery
- Previous history of pseudomembranous colitis, ulcerative colitis, Crohn’s disease, or IBD
- Weakened immunity due to chronic disease, chemotherapy, or immunosuppressant drugs
- Prolonged use of gastric acid suppressants (e.g., proton pump inhibitors)
Pseudomembranous colitis is much less common in children and rare in infants, but is increasingly observed outside the hospital in the community.
Emergence of Aggressive C. difficile Strains
Recently, certain new strains of C. difficile have been reported that:
- Produce significantly more toxins than previous strains
- May be more resistant to some antibiotics
- Affect individuals who haven’t been hospitalized or taken antibiotics
These more virulent strains can cause rapid onset and more severe symptoms, presenting additional treatment challenges.
Complications
While most cases of pseudomembranous colitis are treatable, the condition can become life-threatening if prompt care is not administered, especially in severe cases. The main complications include:
- Severe dehydration from persistent diarrhea
- Toxic megacolon – massive dilation of the colon
- Bowel perforation (a hole in the colon wall)
- Sepsis – a life-threatening body-wide infection
- Acute kidney failure resulting from dehydration
- Death (rare but possible with severe cases)
Complications require immediate medical intervention and can result in hospitalization or intensive care.
Prevention Tips
- Use antibiotics only as prescribed and necessary
- Follow strict hygiene in hospitals and healthcare settings
- Inform healthcare providers of any antibiotic allergies or previous C. difficile infections
- Wash hands thoroughly, especially after restroom use and before eating
- Disinfect common surfaces in healthcare environments regularly
Frequently Asked Questions (FAQs)
Q: What distinguishes pseudomembranous colitis from other forms of colitis?
A: Pseudomembranous colitis is marked by the presence of pseudomembranes—yellow-white plaques visible on colonoscopy, and is most often tied to C. difficile infection following antibiotic use.
Q: Can pseudomembranous colitis develop without taking antibiotics?
A: While antibiotic use is the leading trigger, pseudomembranous colitis can arise in settings of chemotherapy, immunosuppression, or underlying colon diseases, and rare community-acquired cases exist.
Q: How is pseudomembranous colitis diagnosed?
A: Diagnosis typically involves clinical history, stool testing for C. difficile toxins, and sometimes imaging or colonoscopy to visualize pseudomembranes and assess colon inflammation.
Q: What is the prognosis for pseudomembranous colitis?
A: Most people recover fully with prompt treatment, but some cases can be severe and life-threatening if complications such as toxic megacolon or organ failure develop.
Q: Can pseudomembranous colitis recur?
A: Yes, recurrence is possible, particularly if risk factors persist, or if the initial infection was not completely eradicated. Preventive strategies and careful antibiotic stewardship can reduce recurrence risk.
Summary Table: Key Facts about Pseudomembranous Colitis
| Aspect | Details |
|---|---|
| Main Cause | C. difficile infection (most common) |
| Typical Onset | After antibiotics, hospital stay, or immunosuppression |
| Primary Symptoms | Watery diarrhea, abdominal pain, fever, mucus/pus in stool |
| Key Risk Factors | Age >65, recent antibiotics/hospitalization, immunosuppression |
| Complications | Severe dehydration, toxic megacolon, sepsis, kidney failure |
| Prevention | Prudent antibiotic use, infection control in health care settings |
Final Points
Pseudomembranous colitis is a potentially serious colon inflammation predominantly caused by C. difficile after antibiotic use, with symptoms ranging from mild diarrhea to severe, life-threatening complications. Awareness of risk factors and prompt recognition of symptoms can ensure rapid diagnosis and effective treatment, reducing complications and recurrence.
Read full bio of Sneha Tete