Pulmonary Embolism: Diagnosis, Treatment, and Ongoing Care
Comprehensive guide on diagnosing, treating, and managing pulmonary embolism for better patient outcomes.
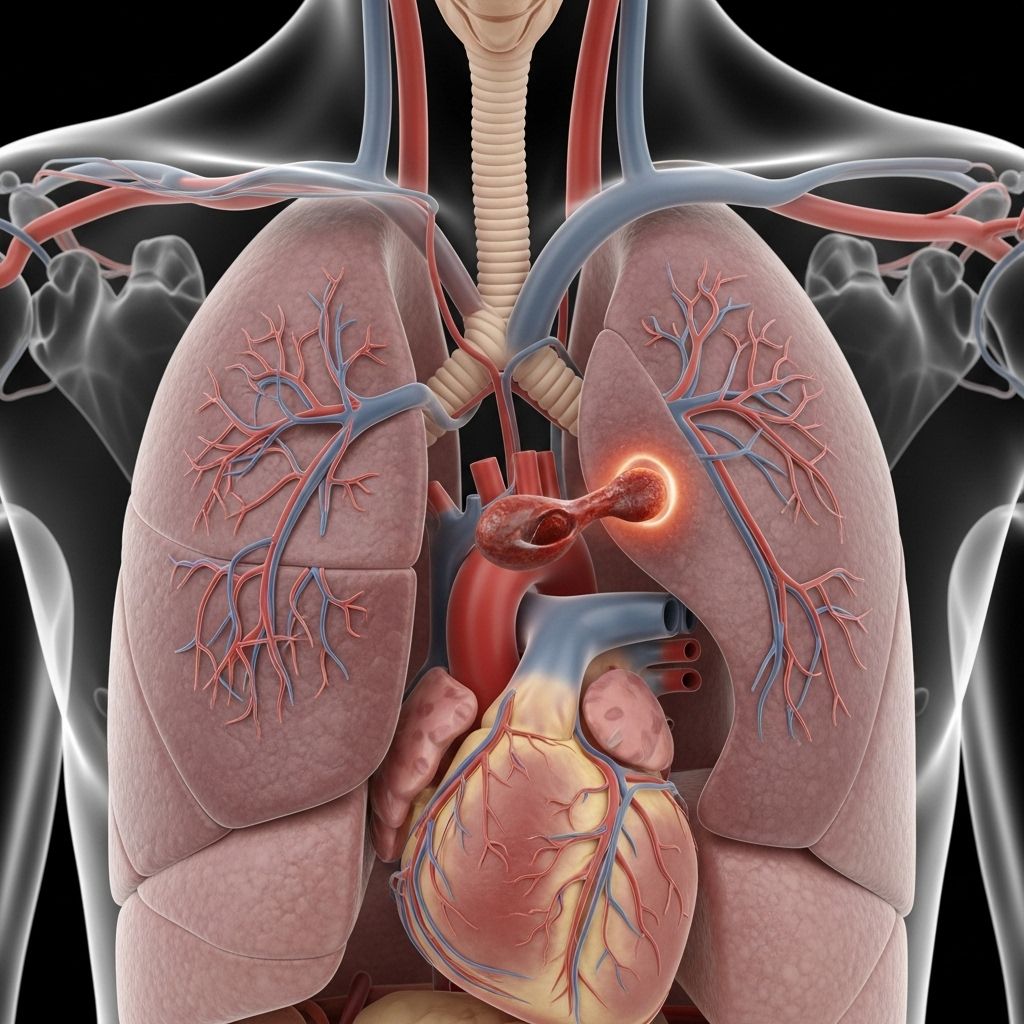
Pulmonary embolism (PE) is a potentially life-threatening condition that occurs when a blood clot blocks an artery in the lungs. Rapid and precise diagnosis followed by targeted treatment can significantly decrease the risk of severe complications and death. This article provides a detailed overview of the essential diagnostic methods, treatment approaches, and measures for ongoing management of pulmonary embolism, synthesizing the latest clinical guidelines and patient care recommendations.
Diagnosis of Pulmonary Embolism
Diagnosing pulmonary embolism is often challenging, particularly for individuals with existing heart or lung illnesses. Accurate diagnosis usually involves a stepwise approach, beginning with a detailed medical history, a thorough physical examination, and a series of specialized diagnostic tests.
Initial Clinical Assessment
- Review of medical history to identify risk factors (recent surgery, prolonged immobilization, previous clotting events).
- Evaluation of symptoms such as sudden shortness of breath, chest pain, rapid heart rate, or unexplained cough.
Core Diagnostic Tests
Depending on individual markers and the clinician’s judgment, several tests may be ordered:
- Blood tests
- Measurement of D dimer levels: Elevated D dimer may indicate the presence of a blood clot but is not specific to pulmonary embolism. Other conditions can also cause high levels.
- Oxygen and carbon dioxide analysis: Blood tests can reveal reduced oxygen levels, indicating impaired lung function due to a clot.
- Inherited clotting disorder screening: If suspected, blood is analyzed to determine if an inherited tendency to clot exists.
- Chest X-ray
- While a chest X-ray cannot diagnose pulmonary embolism directly, it can help exclude other causes of similar symptoms, such as pneumonia or heart failure.
- Ultrasound (Duplex Ultrasonography)
- A noninvasive test, often focusing on the legs, to detect deep vein thrombosis (DVT). The absence of leg clots reduces the likelihood of PE.
- A transducer is passed over the skin to visualize blood flow and detect blockages.
- Other Imaging Techniques
- CT Pulmonary Angiogram: Not always covered in all synopses, but is a gold-standard test for visualizing clots in the lung arteries.
- Ventilation-perfusion (V/Q) scan: May be used when CT is contraindicated or unavailable, by measuring airflow and blood flow in the lungs.
Venogram
In certain cases, a venogram, which involves injecting a dye into a vein and then taking X-ray images, may be employed to assess for the presence of blood clots, particularly in the legs.
Treatment of Pulmonary Embolism
The main goal of treating PE is to prevent the blood clot from increasing in size and to reduce the risk of new clots forming. Prompt and appropriate therapy is vital because untreated pulmonary embolisms carry a high risk of fatality.
Treatment is personalized based on the severity of the clot, the patient’s overall health, and underlying risk factors. It may include medications, invasive procedures, or ongoing management strategies.
Medications
Medication-based treatments for pulmonary embolism primarily involve the use of anticoagulants (blood thinners) and, in specific situations, thrombolytics (clot dissolvers).
- Blood Thinners (Anticoagulants)
- Heparin: Frequently used in hospital settings. Administered either intravenously (IV) or as an injection under the skin, heparin acts quickly to prevent further clot formation.
- Warfarin (Jantovin): An oral anticoagulant often started alongside heparin. It may take several days to reach therapeutic levels, during which continued heparin use is required.
- Direct Oral Anticoagulants (DOACs): Newer medications such as rivaroxaban, apixaban, edoxaban, and dabigatran. They act quickly, do not require preliminary heparin administration, and interact less with other drugs. All anticoagulants can cause bleeding, which is their principal risk.
- Clot Dissolvers (Thrombolytics)
- While most clots resolve with anticoagulant therapy, thrombolytic drugs may be administered in emergency situations involving potentially life-threatening PE. These drugs work to dissolve clots rapidly but can cause sudden, severe bleeding and are reserved for critical situations only.
Surgical and Catheter-Based Procedures
- Clot Removal
- In severe cases, a large clot in the lungs may be physically removed using a flexible catheter inserted through the blood vessels. This technique is typically reserved for patients in a life-threatening situation or when medication is not appropriate.
- Vein Filter (Inferior Vena Cava Filter)
- This approach involves placing a filter in the inferior vena cava (the large vein carrying blood from the lower body to the heart), trapping potential clots before they reach the lungs. It’s reserved for patients who cannot take anticoagulants or who experience clots despite medication. Some filters are designed for removal after the initial risk subsides, while others may remain in place indefinitely.
Hospital Care and Monitoring
Patients with pulmonary embolism are often admitted to the hospital, allowing healthcare teams to monitor for potential complications, adjust medications, and provide close observation during the critical phases of treatment. The severity and location of the clot, along with the patient’s pre-existing conditions, determine the length of stay and intensity of monitoring.
Ongoing Management and Prevention
Managing pulmonary embolism does not end after initial treatment. The risk of recurrence or development of further clots requires a structured ongoing care plan and lifestyle adjustments. Essential components include:
- Continuation of anticoagulant drugs as prescribed, often for several months or longer depending on individual risk.
- Regular follow-up visits for laboratory monitoring and clinical assessment to ensure safe and effective dosing of blood thinners.
- Screening for and addressing underlying risk factors such as inherited clotting disorders, immobility, chronic illness, or cancer.
- Education on recognizing symptoms that may suggest recurrence, such as chest pain, breathing difficulty, or swelling in the limbs.
Lifestyle Modifications to Lower Recurrence Risk
- Staying physically active: Engaging in regular, moderate exercise helps improve circulation and prevent clot formation.
- Maintaining a healthy weight and balanced diet.
- Avoiding extended periods of immobility. During travel or bed rest, flex and extend your legs frequently.
- Wearing compression stockings if recommended, especially for individuals at higher risk of DVT.
Potential Complications and When to Seek Emergency Help
Pulmonary embolism is a medical emergency. Untreated, it can rapidly lead to life-threatening complications, including sudden cardiac arrest or severe lung damage. Approximately 30% of untreated PE cases result in death. Prompt medical attention is crucial for any suspicion of PE to ensure the best possible outcome.
Comparative Table: Diagnostic Tests for Pulmonary Embolism
| Test | Purpose | Advantages | Limitations |
|---|---|---|---|
| Blood Test (D dimer) | Measures clotting activity in blood | Noninvasive, quick | Not specific; may be elevated in other conditions |
| Chest X-ray | Rules out alternative causes of symptoms | Widely available | Cannot confirm PE |
| Ultrasound (Duplex Scan) | Detects DVT, a leading source of PE | Noninvasive, no radiation | Does not confirm PE directly |
| CT Pulmonary Angiogram | Visualizes clots in lung arteries | Highly sensitive and specific | Radiation exposure, not for all patients |
| V/Q Scan | Assesses lung ventilation and blood flow | Useful if CT is contraindicated | Less specific than CT angiogram |
Frequently Asked Questions (FAQs)
What is pulmonary embolism, and why is it dangerous?
Pulmonary embolism is a blockage in a lung artery caused by a blood clot, typically originating from deep veins in the legs. It can significantly impede oxygen flow, causing life-threatening complications if not addressed immediately.
How is a pulmonary embolism diagnosed?
PE is diagnosed using a combination of clinical assessment and various tests, including blood work, chest X-ray, ultrasound, and advanced imaging like CT pulmonary angiography, depending on the case.
What medications are typically used to treat a pulmonary embolism?
The main medications are anticoagulants (blood thinners), such as heparin, warfarin, or newer direct oral anticoagulants. In rare, life-threatening cases, thrombolytic (clot-busting) agents may be used.
Will I need surgery for a pulmonary embolism?
Most patients are treated with medicine, but in some severe cases, a clot may be removed via catheter procedures or surgery. Inferior vena cava filters might be used for patients unable to take blood thinners.
How long will I need treatment, and can pulmonary embolism recur?
Many patients require anticoagulants for several months or longer. Ongoing follow-up and risk reduction strategies are crucial, as there is a risk of recurrence, especially if underlying causes are not addressed.
What are the warning signs that require urgent medical attention?
Sudden chest pain, severe shortness of breath, coughing up blood, rapid heartbeat, and fainting are emergencies demanding immediate care, as they may indicate a new or worsening pulmonary embolism.
How can I reduce the risk of future pulmonary embolisms?
Staying active, avoiding prolonged immobility, managing medical risk factors, and following your healthcare provider’s recommendations for medication and monitoring are the best preventive measures.
Read full bio of medha deb