Pulmonary Fibrosis: Causes, Symptoms, and Key Facts
Understanding the complex causes and symptoms of pulmonary fibrosis, a progressive lung disease characterized by scarring and breathing difficulties.
Pulmonary Fibrosis: Symptoms, Causes, and Essential Facts
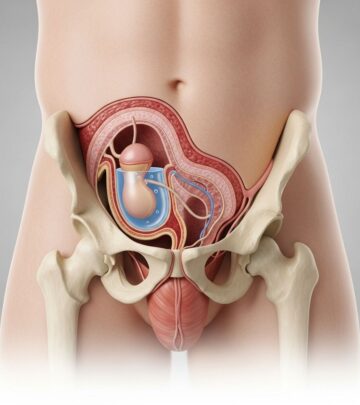
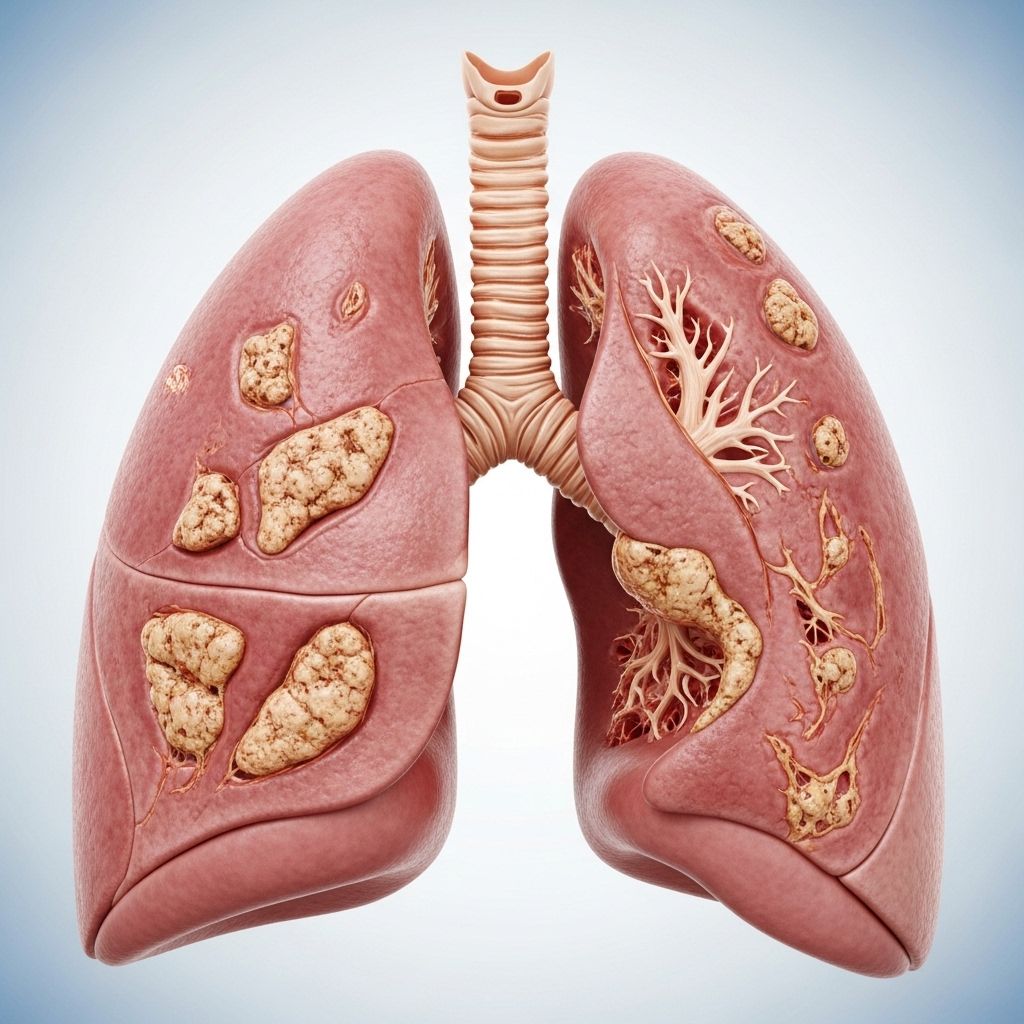
Pulmonary fibrosis is a chronic and progressive lung disease in which the tissue surrounding and between the air sacs (alveoli) in the lungs becomes damaged and scarred. The thickening and stiffening of tissue makes it increasingly difficult for the lungs to work efficiently, leading to reduced oxygen transfer and breathing difficulties.
This article covers the symptoms, causes, risk factors, potential complications, and commonly asked questions about pulmonary fibrosis.
What is Pulmonary Fibrosis?
Pulmonary fibrosis is characterized by the formation of scar tissue in the lungs following damage from various possible sources. The scarring—fibrosis—thickens lung walls, ultimately restricting the lungs’ ability to deliver oxygen to the bloodstream. The lung damage cannot be reversed, but treatments can slow disease progression and help manage symptoms in some cases.
Key Symptoms of Pulmonary Fibrosis
The symptoms experienced by individuals with pulmonary fibrosis can vary and worsen over time. Common symptoms include:
- Shortness of breath (dyspnea), especially during physical exertion.
- Chronic, dry cough.
- Fatigue and weakness.
- Unintended weight loss.
- Aching muscles and joints.
- Chest discomfort or pain.
- Widening and rounding of fingertips or toes, known as clubbing.
Symptoms may worsen gradually over months or years, but some people experience rapid progression. In severe cases, individuals can become breathless even at rest.
Acute Exacerbation: A Sudden Worsening
For some, especially with idiopathic pulmonary fibrosis, symptoms such as shortness of breath can suddenly worsen within days or weeks without a clear cause. This is known as acute exacerbation and can be life-threatening. Illnesses or infections may trigger these events, but often, the exact trigger remains unknown.
When to See a Doctor
- If you experience symptoms such as a persistent cough, shortness of breath, or unexplained weight loss, consult a healthcare professional promptly.
- Seek immediate care if symptoms worsen rapidly.
- Early diagnosis and intervention can help improve the quality of life and potentially slow disease progression.
Causes of Pulmonary Fibrosis
Pulmonary fibrosis can result from multiple factors that damage the lung tissue, but frequently, the specific cause is unknown (“idiopathic pulmonary fibrosis”). Causes fall into several broad categories:
- Environmental and occupational exposures: Long-term or repeated exposure to airborne toxins and pollutants can injure the lungs. Common harmful substances include:
- Silica dust
- Asbestos fibers
- Hard metal dusts
- Wood, coal, or grain dust
- Mold spores
- Bird and animal droppings
- Radiation therapy: Treatment for cancers (such as breast or lung cancer) involving chest radiation can lead to lung damage. The risk and extent of scarring depends on the exposure dose, extent of lung treated, use of chemotherapy, and pre-existing lung conditions.
- Medications: Certain drugs can damage lung tissue as a side effect over long-term use. Examples include some chemotherapy agents, heart medications, antibiotics, and anti-inflammatory drugs.
- Medical conditions: Autoimmune diseases (such as rheumatoid arthritis, scleroderma, and lupus), viral or bacterial lung infections, and interstitial lung disease can cause scarring.
- Unknown cause: In many cases, and particularly in “idiopathic pulmonary fibrosis,” the reason for ongoing lung damage cannot be determined. This form is the most common subtype in adults.
| Cause | Description |
|---|---|
| Environmental & Occupational | Exposure to toxins or particles such as asbestos, silica, grain dust, or animal droppings |
| Radiation Therapy | Chest radiation as treatment for lung/breast cancers damages lung tissue over time |
| Medications | Certain drugs including chemotherapy, heart medications, antibiotics |
| Underlying Diseases | Autoimmune disorders, interstitial lung diseases, infections |
| Idiopathic | No identifiable cause; termed idiopathic pulmonary fibrosis (IPF) |
Risk Factors for Pulmonary Fibrosis
Anyone can develop pulmonary fibrosis, but certain factors increase the risk:
- Age: Most commonly occurs in middle-aged and older adults.
- Sex: Men are more likely to develop idiopathic pulmonary fibrosis than women.
- Exposure to toxins: Working or living in environments with inhaled pollutants increases risk.
- Radiation therapy: Past chest radiation, especially with other treatments, can increase risk.
- Medications: Use of drugs with known pulmonary toxicity.
- Family history: Genetic predispositions may exist; some forms run in families.
- Smoking: Current or former smokers are at a higher risk.
- Pre-existing lung diseases: Having other lung illnesses can predispose to developing fibrosis.
Complications of Pulmonary Fibrosis
Pulmonary fibrosis leads to several serious complications, many of which are life-threatening:
- Pulmonary hypertension: Increased pressure in the lung arteries due to reduced oxygen transfer.
- Respiratory failure: The lungs cannot supply enough oxygen to the body, sometimes requiring ventilatory support.
- Pneumothorax: Collapsed lung caused by rupture in lung tissue.
- Lung cancer: Some types of pulmonary fibrosis increase lung cancer risk over time.
- Acute exacerbations: Sudden, unexplained worsening of symptoms which can be fatal.
How Does Pulmonary Fibrosis Develop?
Normal lung tissue is gradually replaced by fibrotic (scarred) tissue following tissue damage and abnormal wound healing.
- This process restricts lung expansion and decreases oxygen diffusion.
- Pulmonary fibrosis is primarily driven by irregular wound healing rather than persistent inflammation.
- Several genes and cell signaling pathways contribute to the development and progression of lung scarring, including TGF-β, CTGF, EGFR, IL-13, PDGF, and Wnt/β-catenin.
Genetic and Molecular Influences
- TGF-β: Stimulates scar tissue formation.
- CTGF: Promotes extracellular matrix production and remodeling.
- EGFR: Regulates cell growth; its dysregulation contributes to fibrosis.
- IL-13 and PDGF: Encourage recruitment of fibroblasts and new tissue formation.
- Wnt/β-catenin and chromatin remodeling: Affect gene expression involved in tissue repair and scarring.
Who Is Affected by Pulmonary Fibrosis?
- Affects more than 5 million people worldwide.
- Most cases appear in people aged 50 and older, but it can occasionally develop in children or infants.
- Idiopathic pulmonary fibrosis is most common in adults, especially men.
- No clear cure; focus remains on symptom management and slowing disease progression.
When Should You Seek Medical Help?
- If you have persistent respiratory symptoms (breathlessness, cough), seek evaluation promptly.
- If symptoms worsen suddenly, call your healthcare provider immediately, as you may be experiencing an acute exacerbation.
- Early diagnosis enables intervention strategies to improve quality of life.
Living With Pulmonary Fibrosis
- No cure exists for pulmonary fibrosis; lung tissue damage is not reversible.
- Treatments focus on slowing progression, alleviating symptoms, and improving everyday functioning.
- Therapies may include oxygen supplementation, pulmonary rehabilitation, certain medications, and in advanced cases, lung transplantation.
Frequently Associated Risk Factors Table
| Risk Factor | Details |
|---|---|
| Age | Primarily affects adults over 50 |
| Sex | More common in men |
| Environmental Exposure | Occupational or residential exposure to pollutants or toxins (asbestos, silica, etc.) |
| Genetic Factors | Family history of lung disease |
| Pre-existing Disease | Autoimmune diseases and other types of interstitial lung disease |
| Medications | Long-term use of chemotherapy, antibiotics, heart medications |
| Smoking | Current and former tobacco use |
| Radiation Therapy | Past chest radiotherapy |
Frequently Asked Questions (FAQs)
Q: Is pulmonary fibrosis curable?
A: Pulmonary fibrosis cannot be cured. Treatments can alleviate symptoms and help slow the disease, but damage to the lungs is permanent.
Q: How is pulmonary fibrosis different from other lung diseases?
A: Pulmonary fibrosis primarily involves scarring of the lung tissue, leading to stiffness and impaired oxygen transfer. Other lung diseases may involve different processes, such as airway obstruction or chronic infection.
Q: Can young people get pulmonary fibrosis?
A: While it most often affects adults, especially those over 50, pulmonary fibrosis can rarely occur in children or infants.
Q: What are the first signs of pulmonary fibrosis?
A: Initial symptoms include shortness of breath with exertion, dry cough, and fatigue. These signs often progress over time, becoming more pronounced.
Q: What should I do if my symptoms suddenly get worse?
A: Seek medical help immediately if you experience a sudden worsening of breathlessness or other symptoms. Acute exacerbations can be dangerous and require prompt treatment.
Q: What are the main risk factors I should be aware of?
A: Age, sex, environmental exposures, family history, underlying health conditions, medications, and smoking are all key risk factors for developing pulmonary fibrosis.
Q: What lifestyle changes can help manage pulmonary fibrosis?
A: Avoid exposure to lung irritants, follow prescribed therapies, participate in pulmonary rehab if recommended, and maintain open communication with your healthcare team. Quitting smoking is especially important.
Key Takeaways
- Pulmonary fibrosis is a chronic lung disorder marked by progressive scarring and loss of lung function.
- Symptoms primarily include shortness of breath, cough, fatigue, and clubbing of fingers.
- Multiple causes exist, but in most cases, the source remains unknown.
- Risk factors include age, environmental exposure, medications, smoking, and family history.
- Complications are serious and include pulmonary hypertension, respiratory failure, and increased risk of lung cancer.
- No cure exists; treatment focuses on managing symptoms and improving quality of life.
- Prompt medical attention and ongoing management are crucial for preserving lung function and well-being.
References
- https://en.wikipedia.org/wiki/Pulmonary_fibrosis
- https://www.mayoclinic.org/diseases-conditions/cystic-fibrosis/symptoms-causes/syc-20353700
- https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis/symptoms-causes/syc-20353690
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/pulmonary-fibrosis
- https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis/diagnosis-treatment/drc-20353695
- https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis/care-at-mayo-clinic/mac-20353699
- https://www.mayoclinic.org/diseases-conditions/interstitial-lung-disease/symptoms-causes/syc-20353108
- https://www.amerikanhastanesi.org/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/pulmonary-fibrosis
- https://www.youtube.com/watch?v=aCJJz8le5Tk
Read full bio of medha deb