Sciatica: Diagnosis, Treatment, and Recovery Strategies
Learn comprehensive methods for diagnosing, treating, and recovering from sciatica, including medical and self-care strategies.
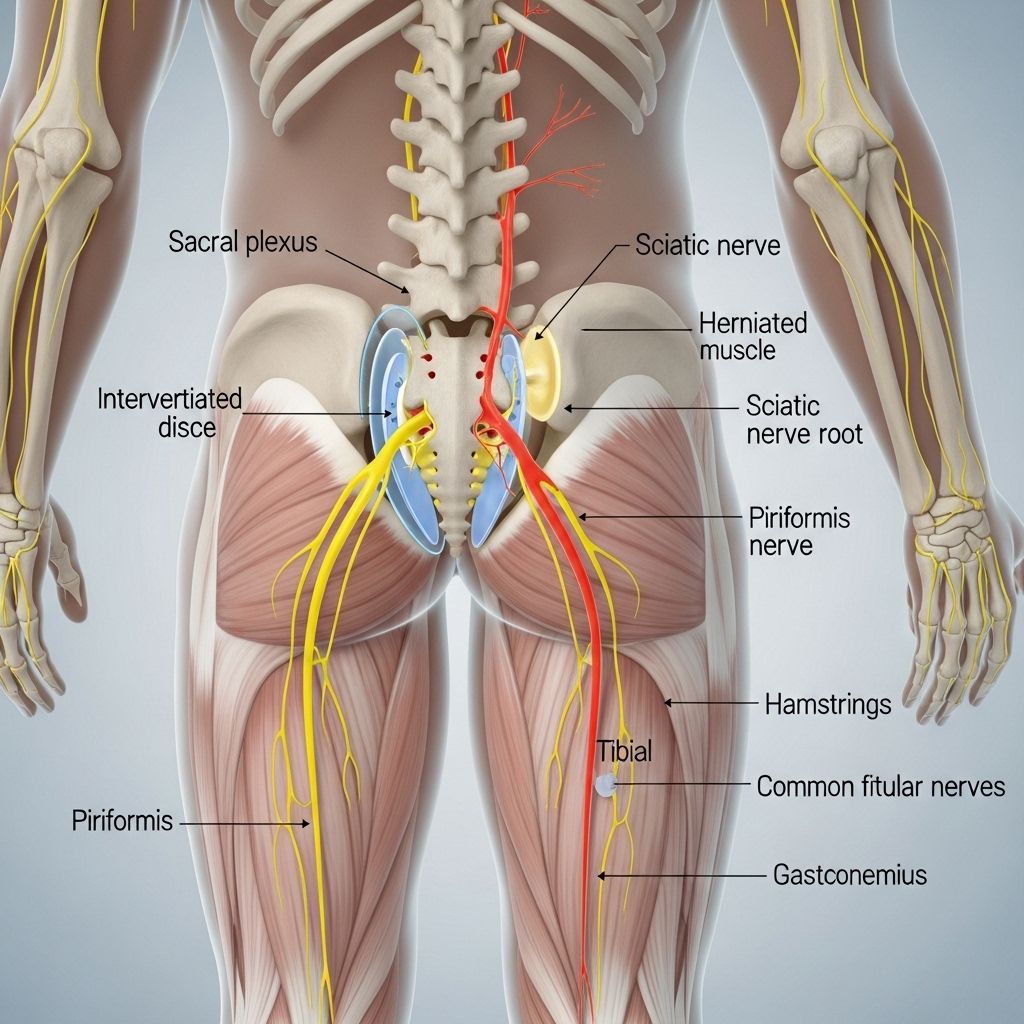
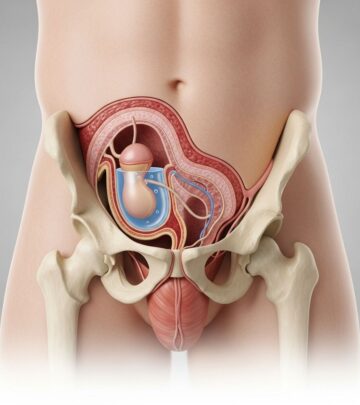
Sciatica refers to pain that travels along the sciatic nerve, typically radiating from the lower back through the hips and buttocks and down one leg. This condition can deeply impact day-to-day life, causing not only pain but also numbness, tingling, or weakness in the affected limb. Timely diagnosis and appropriate interventions are crucial to managing symptoms and restoring function. This guide provides a comprehensive overview of sciatica diagnosis, treatment options, self-care strategies, and offers answers to common questions.
Diagnosis
Effective management begins with an accurate diagnosis of sciatica and its underlying cause. Health professionals employ a combination of physical examination and diagnostic tests to determine the severity and origin of nerve compression.
Physical Examination
- Muscle strength and reflexes: Your doctor may ask you to walk on your toes or heels, rise from a squatting position, or lift your leg while lying down. These maneuvers help detect nerve involvement and muscle weakness.
- Neurological assessment: This includes checking your response to sensations and reflexes to ascertain which nerve may be affected.
Diagnostic Tests
Imaging and electrical studies are recommended for patients with severe pain or symptoms that do not improve within a few weeks:
- X-ray: Reveals structural changes in the spine and may highlight bone spurs or disc degeneration.
- MRI: Utilizes strong magnets and radio waves to generate detailed images of soft tissues. MRI can show herniated disks and pinched nerves with high clarity.
- CT scan: May include injection of a dye into the spinal canal (CT myelogram), which helps visualize spinal cord and nerve roots.
- Electromyography (EMG): Assesses electrical activity in muscles and reveals the presence and severity of nerve root injury.
Treatment
Treatment for sciatica depends on severity, duration, and underlying cause. Most cases improve with conservative measures, though persistent or worsening symptoms may require medical intervention.
Self-Care Techniques
- Cold packs: Apply to painful areas for about 20 minutes, several times daily, especially useful in the initial days to reduce inflammation.
- Heat therapy: After two to three days, use heating pads on a low setting or a heat lamp to soothe muscle tension.
- Alternating hot and cold: Switching between heat and cold may provide further relief.
- Gentle activity modification: Avoid excessive bending, lifting, or twisting. Adjust activities to minimize strain on the lower back.
Medications
For patients with persistent pain, several pharmaceutical options are available:
- Anti-inflammatories: Over-the-counter NSAIDs (e.g., ibuprofen) help manage pain and inflammation.
- Corticosteroids: Provide potent anti-inflammatory effects, either orally or by injection.
- Antidepressants: Some types can help modulate chronic pain.
- Anti-seizure medications: Gabapentin and pregabalin are commonly used for nerve pain.
- Opioids: May be used for severe pain, but typically reserved due to risk of dependence.
Physical Therapy
Once acute pain subsides, guided exercises and therapy promote healing and help prevent future episodes:
- Strengthening core muscles: Core stability reduces pressure on the spine.
- Range of motion exercises: Stretching and flexibility routines minimize stiffness.
- Posture correction: Training to improve posture limits undue stress on spinal structures.
- Exercise recommendations: Therapists design individualized routines to address weak areas.
Steroid Injections
- Epidural corticosteroid injection: Reduces inflammation around the nerve root. Often, a single injection can provide substantial relief; up to three injections per year may be recommended.
Surgical Options
- Discectomy: Removal of the herniated part of a disc compressing the nerve.
- Laminectomy: Removal of bone spurs or segments of bone overlying the nerve.
- Surgery indications: Reserved for cases with severe muscle weakness, loss of bowel or bladder control, or pain that does not respond to other treatments.
When to Seek Medical Attention
- Persistent or severe pain: Consult your healthcare provider if pain worsens or isn’t relieved by over-the-counter medications and rest.
- Recent trauma: If pain follows an accident or significant fall, prompt evaluation is needed to rule out serious spinal injuries.
- Signs of infection: Fever, chills, and night sweats warrant immediate medical review.
- Cancer history: Previous or current cancer requires careful assessment of new sciatica symptoms.
- Loss of muscle control: Sudden problems with walking or control of bowel/bladder are medical emergencies.
Recovery and Ongoing Care
Most cases of sciatica improve with time and conservative treatments. Long-term management focuses on preventing recurrence and supporting recovery through healthy lifestyle choices.
- Activity as tolerated: Gentle movement, such as walking and stretching, aids healing.
- Home exercise program: Continue exercises outlined by your physical therapist.
- Weight management: Maintaining a healthy weight reduces the risk of further nerve compression.
- Healthy posture: Regular attention to alignment protects the spine.
Departments & Specialists Treating Sciatica
- Neurology
- Pain Rehabilitation Centers
- Pediatric Pain Rehabilitation Centers
- Physical Medicine and Rehabilitation
- Spine Care
Collaborative care from these departments ensures thorough evaluation and treatment plans tailored to each patient’s needs.
Frequently Asked Questions (FAQs)
Q: What causes sciatica?
A: Sciatica usually results from a herniated disk, bone spur, or spinal stenosis that compresses the nerve roots forming the sciatic nerve.
Q: How long does sciatica pain last?
A: Sciatica is often intensely painful for one to two weeks but gradually improves with conservative management in most cases.
Q: Can sciatica resolve without surgery?
A: Yes, about 90% of sciatica cases respond well to non-surgical measures including medications, physical therapy, and activity modification.
Q: What self-care strategies can I use at home?
A: Apply heat or cold packs, avoid activities that worsen pain, use over-the-counter pain relievers, and remain moderately active.
Q: When is surgery necessary?
A: Surgery is considered when there is severe, unremitting pain, muscle weakness, or loss of bowel or bladder control, or when non-surgical approaches fail to provide relief.
Q: Are alternative therapies useful?
A: Some individuals benefit from complementary therapies such as acupuncture, massage, yoga, or chiropractic adjustments. However, always consult a healthcare professional before starting these, especially if your symptoms are severe.
Sciatica Pain Management Table
| Treatment Option | Purpose | Typical Indications | Common Side Effects |
|---|---|---|---|
| NSAIDs / Anti-inflammatories | Pain and inflammation relief | Mild to moderate pain, initial therapy | GI upset, ulcers with prolonged use |
| Steroids (oral/injections) | Reduce nerve inflammation | Moderate to severe pain, failed NSAIDs | Weight gain, blood sugar changes |
| Antidepressants/Antiseizure | Target nerve pain | Chronic or neuropathic pain syndromes | Drowsiness, dry mouth, dizziness |
| Opioids | Severe pain | Pain unresponsive to other medications | Constipation, drowsiness, dependency risk |
| Physical Therapy | Restore movement, prevent recurrence | After acute pain subsides | Very few; initial soreness possible |
| Surgery | Remove cause of nerve compression | Refractory pain, weakness, bowel/bladder loss | Operative risks, recovery time |
Tips for Preventing Sciatica Recurrence
- Follow regular strengthening and stretching routines.
- Maintain healthy posture at work and home.
- Lift objects properly using your legs, not your back.
- Maintain a healthy weight to reduce spinal stress.
- Use supportive chairs when sitting for extended periods.
Summary
Sciatica presents a wide spectrum of symptoms, from mild discomfort to intense, disabling pain. Most cases are managed successfully using conservative treatments, medications, and physical therapy. Surgery is rarely required but can be highly effective when indicated. The best outcomes are achieved through early diagnosis, tailored treatment, and long-term preventative strategies. For any concerning symptoms, especially those impacting mobility or basic body functions, consult a healthcare provider without delay.
Read full bio of Sneha Tete