Thrombocytosis: Understanding High Platelet Counts, Symptoms, and Causes
Explore what causes thrombocytosis, its symptoms, and how it differs between primary and secondary types.
Thrombocytosis: Symptoms, Causes, and Types
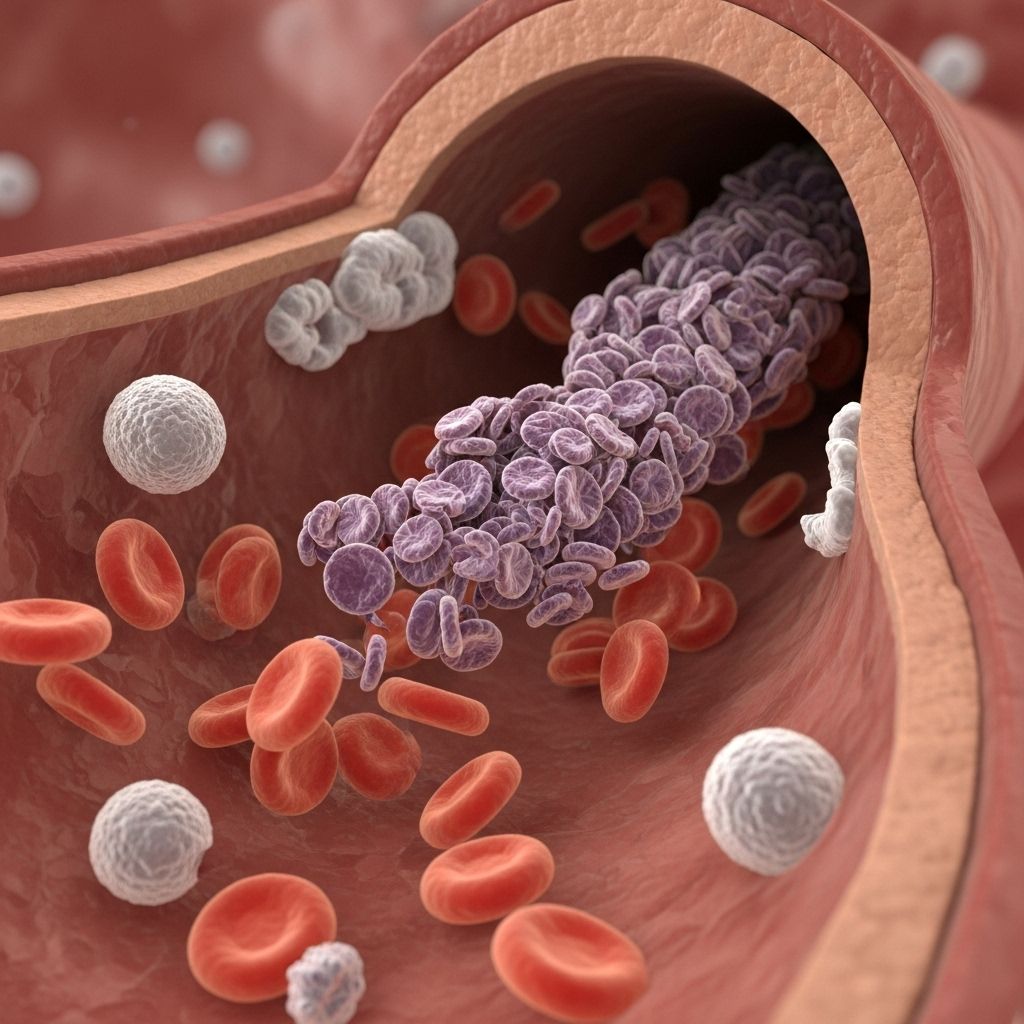
Thrombocytosis is a blood disorder characterized by an abnormally high number of platelets, the blood cells responsible for helping blood clot. While often detected incidentally through blood tests, this condition can sometimes lead to serious complications such as blood clots or abnormal bleeding. Understanding thrombocytosis, its symptoms, underlying causes, and the different types is crucial for effective management and treatment.
Overview
Platelets, also known as thrombocytes, are small cell fragments in the blood produced by bone marrow. Their primary role is to stop bleeding by clumping and forming plugs in blood vessel injuries. In thrombocytosis, the body produces too many platelets, raising the risk of abnormal blood clotting or, less commonly, bleeding episodes.
There are two main types of thrombocytosis based on their cause:
- Reactive thrombocytosis (also known as secondary thrombocytosis)
- Essential thrombocythemia (also called primary thrombocytosis)
Distinguishing the type of thrombocytosis is critical in clinical practice because it directs appropriate diagnostic and treatment strategies.
Types of Thrombocytosis
| Type | Description | Main Causes | Complication Risk |
|---|---|---|---|
| Reactive Thrombocytosis | Elevation in platelet count as a response to another condition. | Infections, inflammation, trauma, blood loss, surgery, iron deficiency, cancer, some medications. | Lower risk of serious complications. |
| Essential Thrombocythemia (Primary) | Disorder of the bone marrow, causing excessive production of platelets without an underlying external trigger. | Genetic mutations in bone marrow stem cells; commonly JAK2, CALR, or MPL mutations. | Higher risk of clotting, bleeding, and other complications. |
Reactive (Secondary) Thrombocytosis
This form of thrombocytosis is far more common. It arises as a reaction to another medical condition or event—such as infection, recent surgery, inflammation, trauma, or even some medications. Because the elevated platelet count is due to an external cause, treating the underlying issue often returns platelet counts to normal.
Essential Thrombocythemia (Primary Thrombocytosis)
Essential thrombocythemia is a bone marrow disorder arising from genetic changes in the bone marrow stem cells. These mutations prompt uncontrolled proliferation of platelets, which may malfunction. Essential thrombocythemia is rarer, typically affects adults over 50, and is associated with a greater risk of both clotting (thrombosis) and bleeding. It is considered one of the myeloproliferative neoplasms—a group of blood cancers.
Symptoms
Most people with thrombocytosis, especially the reactive type, do not experience symptoms and are diagnosed after routine blood tests. When symptoms are present, they often stem from abnormal clotting or, less commonly, bleeding.
Common Symptoms of Thrombocytosis
- Headache
- Confusion or changes in speech
- Chest pain
- Shortness of breath and nausea
- Weakness
- Burning pain in the hands or feet
These symptoms often relate to the formation of small blood clots in blood vessels, which can impair blood flow to various organs.
Symptoms Caused by Bleeding (Less Common)
- Nosebleeds
- Bruising easily
- Bleeding from the gums or mouth
- Blood in stool
In rare situations, particularly when platelet counts are extremely high or platelets are dysfunctional, paradoxical bleeding rather than clotting can occur.
When to See a Doctor
Since thrombocytosis is frequently asymptomatic, it is often detected incidentally. Anyone experiencing unexplained symptoms such as headache, persistent chest pain, vision changes, recurrent bruising, or abnormal bleeding should seek prompt medical evaluation.
Causes
The main factors contributing to a high platelet count depend on the type of thrombocytosis.
Causes of Reactive (Secondary) Thrombocytosis
- Acute or chronic infections
- Acute or chronic inflammation (e.g., rheumatoid arthritis)
- Iron deficiency, especially in children
- Cancer
- Surgical procedures or trauma (including broken bones, wounds)
- Splenectomy (removal of the spleen)
- Certain medications (such as corticosteroids)
- Hemorrhage (significant blood loss)
Reactive thrombocytosis usually resolves as the underlying issue is treated or heals.
Causes of Essential Thrombocythemia (Primary)
- Genetic mutations in bone marrow stem cells; commonly the JAK2, CALR, or MPL genes.
- No readily identifiable external trigger or condition.
The exact mechanisms behind these genetic mutations are still under investigation. Essential thrombocythemia is considered a blood and bone marrow disease and may be classified alongside other myeloproliferative neoplasms.
Risk Factors
- Age: Essential thrombocythemia is more common in adults over 50 years old.
- Sex: Women are slightly more likely to develop essential thrombocythemia than men.
- History of underlying conditions: Infections, chronic inflammation, or iron deficiency increase risk for reactive thrombocytosis.
- Genetic predisposition: Family history of myeloproliferative neoplasms may increase risk.
There are generally no lifestyle-related risk factors linked to thrombocytosis, particularly the essential type.
Complications
Most individuals with mild or reactive thrombocytosis experience no serious complications. However, essential thrombocythemia and severe cases of thrombocytosis can lead to significant health concerns.
Blood Clotting (Thrombosis)
- Increased risk of forming abnormal blood clots (thrombi), which can block blood flow.
- Clotting events may occur in the brain (stroke), heart (heart attack), lungs (pulmonary embolism), legs (deep vein thrombosis), or smaller vessels of fingers and toes.
- Clots in placental or uterine blood vessels can complicate pregnancy.
Bleeding
- Very high or dysfunctional platelet counts can paradoxically result in bleeding rather than clotting.
- Symptoms include nosebleeds, gastrointestinal bleeding, bloody stools, or bleeding gums.
Other Complications (Rare)
- Progression to other blood disorders, such as myelofibrosis (bone marrow scarring) or acute leukemia.
- In advanced cases, essential thrombocythemia may lead to bone marrow complications or transformation into myelodysplastic syndrome or acute leukemia.
Diagnosis
Thrombocytosis is usually discovered during routine blood testing. The key steps in diagnosis include:
- Complete blood count (CBC): Determines platelet levels and screens for other abnormalities.
- Assessment for underlying causes (medical history, physical examination, other laboratory studies).
- Bone marrow tests or genetic testing (for suspected essential thrombocythemia).
Distinguishing reactive from essential thrombocytosis is crucial. Consulting a hematologist (blood specialist) is often recommended, particularly when platelet counts are very high or no secondary cause is found.
When to Seek Immediate Medical Attention
- Sudden, severe headache or neurological changes (confusion, difficulty speaking)
- Intense chest pain or shortness of breath
- Signs of stroke, heart attack, or severe bleeding
Prevention
There are no proven strategies to prevent essential thrombocythemia, as most cases result from spontaneous genetic mutations. For reactive thrombocytosis, controlling or promptly treating underlying infections, inflammation, or other medical conditions can reduce risk.
Frequently Asked Questions (FAQs)
Q: What is a normal platelet count?
A: Typical platelet counts in adults range from 150,000 to 450,000 per microliter of blood. Counts above this are considered thrombocytosis.
Q: What are the most common causes of a high platelet count?
A: The majority are due to reactive (secondary) thrombocytosis, which is a response to infections, inflammation, recent surgery, trauma, or iron deficiency. Essential (primary) thrombocytosis is less common and caused by bone marrow mutations.
Q: If I have a high platelet count, does it mean I have cancer?
A: Not necessarily. Most cases are not caused by cancer and are instead reactive to another medical issue. Essential thrombocythemia, one type, is considered a myeloproliferative neoplasm (a form of blood cancer) but is different from other types such as leukemia.
Q: Can thrombocytosis cause symptoms even if I feel healthy?
A: Many people with thrombocytosis are asymptomatic and may never develop symptoms. However, some can experience complications if blood clots or bleeding develop unexpectedly.
Q: How is the cause of thrombocytosis determined?
A: Doctors use a combination of blood tests, review of medical history, assessment of underlying medical conditions, and sometimes bone marrow examination or genetic testing.
Q: What are the treatment options for thrombocytosis?
A: Treatment depends on the underlying cause. For reactive thrombocytosis, addressing the primary condition usually resolves high platelet counts. Essential thrombocythemia may require medications to lower platelet numbers and reduce clotting or bleeding risk.
Q: Is thrombocytosis dangerous during pregnancy?
A: Essential thrombocythemia can raise the risk of pregnancy complications such as miscarriage or placental blood clots. Close monitoring and specialized care may be needed.
Key Takeaways
- Thrombocytosis indicates an abnormally high platelet count.
- It is classified as reactive (secondary) or essential (primary), based on its cause.
- Most people are asymptomatic; when symptoms occur, they are mainly due to blood clots or, less commonly, bleeding.
- Diagnosis relies on blood tests and, sometimes, bone marrow and genetic studies.
- Consult a healthcare provider if you have unexplained symptoms or a persistently high platelet count.
Read full bio of Sneha Tete