Uterine Fibroids: Symptoms, Causes, and Key Insights
Understand the causes, symptoms, risk factors, complications, and prevention of uterine fibroids, a common noncancerous growth in women.
Uterine fibroids are noncancerous growths that develop in or on the uterus during a woman’s reproductive years. Despite their benign nature, these growths—also known as leiomyomas or myomas—can greatly impact quality of life or sometimes remain entirely unnoticed. This comprehensive overview explores what uterine fibroids are, their signs and symptoms, causes and risk factors, potential complications, and strategies for prevention.
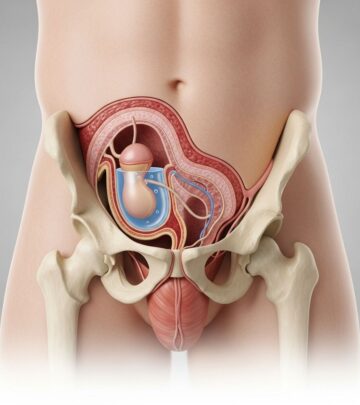
What Are Uterine Fibroids?
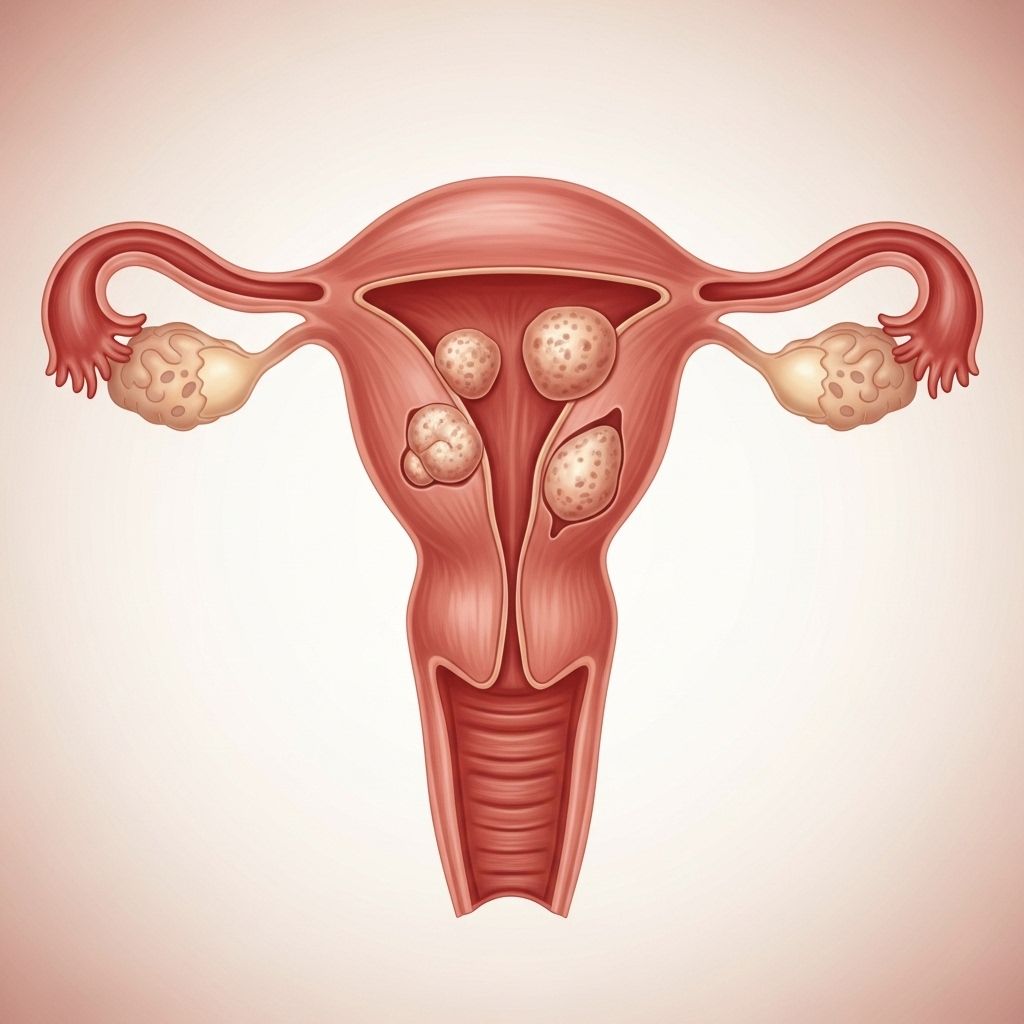
Uterine fibroids are firm, rubbery masses formed from the muscle and connective tissue of the uterus. Ranging from tiny, undetectable seedlings to large masses that enlarge the uterus, fibroids can develop as a single nodule or as clusters of various sizes. The number and size of fibroids can vary significantly from person to person, and their presence does not necessarily indicate a medical problem or cancer risk.
Fibroids are classified based on their location within or on the uterus:
- Intramural fibroids: Grow within the muscular uterine wall.
- Submucosal fibroids: Bulge into the uterine cavity.
- Subserosal fibroids: Project to the outside of the uterus.
Many women have uterine fibroids during their lifetimes, especially between the ages of 30 and 40. Despite this, most women do not experience symptoms and may discover fibroids incidentally during a pelvic exam or prenatal ultrasound.
Symptoms
While most fibroids are asymptomatic, some women experience symptoms influenced by the number, size, and location of the fibroids. These symptoms can vary from mild discomfort to severe, life-disrupting problems.
Common Signs and Symptoms
- Heavy menstrual bleeding: Sometimes requiring pad or tampon changes every hour, lasting more than a week, or featuring large blood clots.
- Prolonged menstrual periods: Lasting longer than usual.
- Pelvic pressure or pain: Persistent feelings of fullness or discomfort in the lower abdomen.
- Frequent urination: Due to pressure on the bladder.
- Difficulty emptying the bladder: Sensation of incomplete urination.
- Constipation: Pressure on the bowel can impair regular movements.
- Backache or leg pains: Especially if fibroids press on nerves.
Rarely, a fibroid may outgrow its blood supply, causing sudden, acute pain as the tissue begins to die.
When to See a Health Care Provider
- Persistent pelvic pain or sudden sharp pelvic pain
- Heavy, prolonged, or painful periods
- Spotting or bleeding between periods
- Difficulty emptying the bladder
- Unexplained low red blood cell count (anemia)
- Severe vaginal bleeding that does not stop
Early evaluation is important to identify fibroids and rule out other serious conditions.
Causes
The precise cause of uterine fibroids is still being researched. However, a combination of genetic, hormonal, and growth factors appears to play a role in their development.
- Genetics: Many fibroids contain genetic changes distinct from normal uterine muscle tissue. There is also a higher risk if you have a family history of fibroids.
- Hormones: Estrogen and progesterone, two key hormones that regulate the menstrual cycle, appear to promote fibroid growth.
- Other growth factors: Substances that help the body maintain tissues, such as insulin-like growth factor, may also contribute.
Fibroids tend to shrink after menopause, likely due to decreased hormone production.
Risk Factors
Although any woman of reproductive age can develop uterine fibroids, certain factors increase the risk:
- Age: Most common in women 30–40 years old before menopause.
- Family history: Having a mother or sister with fibroids increases your risk.
- Race: Women of African descent are at higher risk and may develop fibroids at a younger age with more severe symptoms.
- Obesity: Higher body weight may increase fibroid risk.
- Diet: High intake of red meat and low vegetable consumption may play a role.
- Early menstruation: Starting periods at an early age is linked to increased risk.
- Vitamin D deficiency, alcohol use, and birth control use have variable impacts according to current research.
Despite these risk factors, many women with no apparent risks still develop fibroids.
Complications
While most fibroids are harmless, some can lead to complications that may impact daily life or future reproductive health:
- Anemia: Heavy menstrual bleeding can cause iron deficiency anemia, leading to fatigue and weakness.
- Severe pain: Particularly if a fibroid loses its blood supply.
- Fertility and pregnancy concerns: Certain fibroids distort the uterine cavity or block the fallopian tubes, which can complicate conception or pregnancy, potentially causing miscarriage or early labor.
- Pressure effects: Large fibroids can compress the bladder, ureters, or rectum, causing urinary or bowel issues.
Very rarely, a rapidly growing mass may be a type of cancerous tumor called a leiomyosarcoma, but this is exceedingly uncommon. Fibroids themselves almost never become cancerous.
Prevention
While there is no guaranteed way to prevent uterine fibroids, certain lifestyle adjustments may reduce risk or help manage symptoms:
- Maintain a healthy weight: Regular exercise and a balanced diet may lower the risk.
- Eat fruits and vegetables: High consumption of leafy greens and low intake of red meat may be protective.
- Monitor blood pressure: Some studies associate elevated blood pressure with fibroid risk.
- See your healthcare provider: Routine checkups can identify fibroids early, especially if there is family history or risk factors present.
There is currently no medical consensus or specific actions proven to definitively prevent fibroids.
Diagnosis
Fibroids are often discovered incidentally during routine gynecologic exams or pregnancy ultrasounds. To confirm the diagnosis and assess size, number, and location, your healthcare provider may use several tools:
- Pelvic exam: Palpating the uterus for irregularities.
- Ultrasound: Imaging using sound waves to create a picture of the uterus.
- Magnetic resonance imaging (MRI): Especially useful for mapping and sizing fibroids.
- Other imaging: Hysterosonography (saline infusion ultrasound), hysterosalpingography (dye X-ray), or hysteroscopy (camera through cervix).
- Blood tests: To check for anemia or rule out other causes of abnormal bleeding.
The choice of diagnostic tool depends on personal medical history, symptoms, and reproductive plans.
Types of Uterine Fibroids
| Type | Location | Typical Symptoms |
|---|---|---|
| Intramural | Within the uterine wall | Heavy bleeding, pelvic pain |
| Submucosal | Beneath uterine lining, projects into the cavity | Bleeding, fertility issues |
| Subserosal | Outer wall of uterus | Pressure symptoms, frequent urination |
Living with Uterine Fibroids
Most people with fibroids do not experience symptoms and may not require treatment. For those who do, fibroid-related issues can disrupt physical, emotional, and reproductive health. It’s important to have regular communication with your healthcare provider to monitor fibroid size and discuss treatment options if symptoms worsen or affect your well-being.
Frequently Asked Questions (FAQs)
What causes uterine fibroids to grow?
While the exact cause remains unclear, hormones such as estrogen and progesterone, genetic factors, and certain lifestyle factors (such as diet and stress) influence fibroid growth. Fibroids tend to increase during years when hormone levels are highest and shrink after menopause.
Are uterine fibroids cancerous?
No, uterine fibroids are almost always benign (noncancerous). Malignant transformation (cancer) is extremely rare.
Who is at greatest risk for uterine fibroids?
Fibroids are most common in women aged 30 to 40. Women of African descent, those with a family history, obesity, or early onset of menstruation have increased risk.
Can I get pregnant if I have fibroids?
Most women with fibroids can conceive normally. However, some fibroids may interfere with implantation or increase miscarriage risk, especially if they distort the uterine cavity.
When should I worry about my fibroids?
You should see a healthcare provider if you experience pelvic pain, heavy or prolonged bleeding, unexplained anemia, or difficulty with urination or bowel movements.
What are treatment options for uterine fibroids?
Treatment depends on symptoms, size, location, and reproductive plans. Options include watchful waiting (for small or asymptomatic fibroids), medical therapies (hormonal and non-hormonal), minimally invasive procedures (like uterine artery embolization), and surgical interventions (myomectomy or hysterectomy).
Key Takeaways
- Uterine fibroids are the most common benign tumors affecting the female reproductive system.
- Symptoms range from none at all to heavy bleeding, pain, and pressure effects.
- Risk is increased with age, family history, race, and certain lifestyle factors.
- Diagnosis is typically via pelvic exam and imaging studies.
- Treatment varies and should be individualized based on symptoms and plans for future fertility.
If you have concerns about uterine fibroids or experience any related symptoms, consult your healthcare provider for evaluation and possible management options.
References
- https://newsnetwork.mayoclinic.org/discussion/womens-wellness-uterine-fibroids-are-common-noncancerous-growths/
- https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-risk-factors-for-uterine-fibroids/
- https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-what-are-fibroids/
- https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
- https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/multimedia/vid-20538085
- https://www.mayoclinic.org/departments-centers/fibroid-clinic/overview/ovc-20508774
- https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294
- https://www.youtube.com/watch?v=u3l3HMJmk_0
- https://www.youtube.com/watch?v=oY9Hw3FjdrA
Read full bio of Sneha Tete