Anal Fissures: Symptoms, Causes, Diagnosis, and Treatments
Comprehensive guide to anal fissures: uncover symptoms, causes, diagnosis, and advanced treatment approaches.
Anal Fissures: Understanding, Diagnosing, and Managing a Common Anorectal Condition
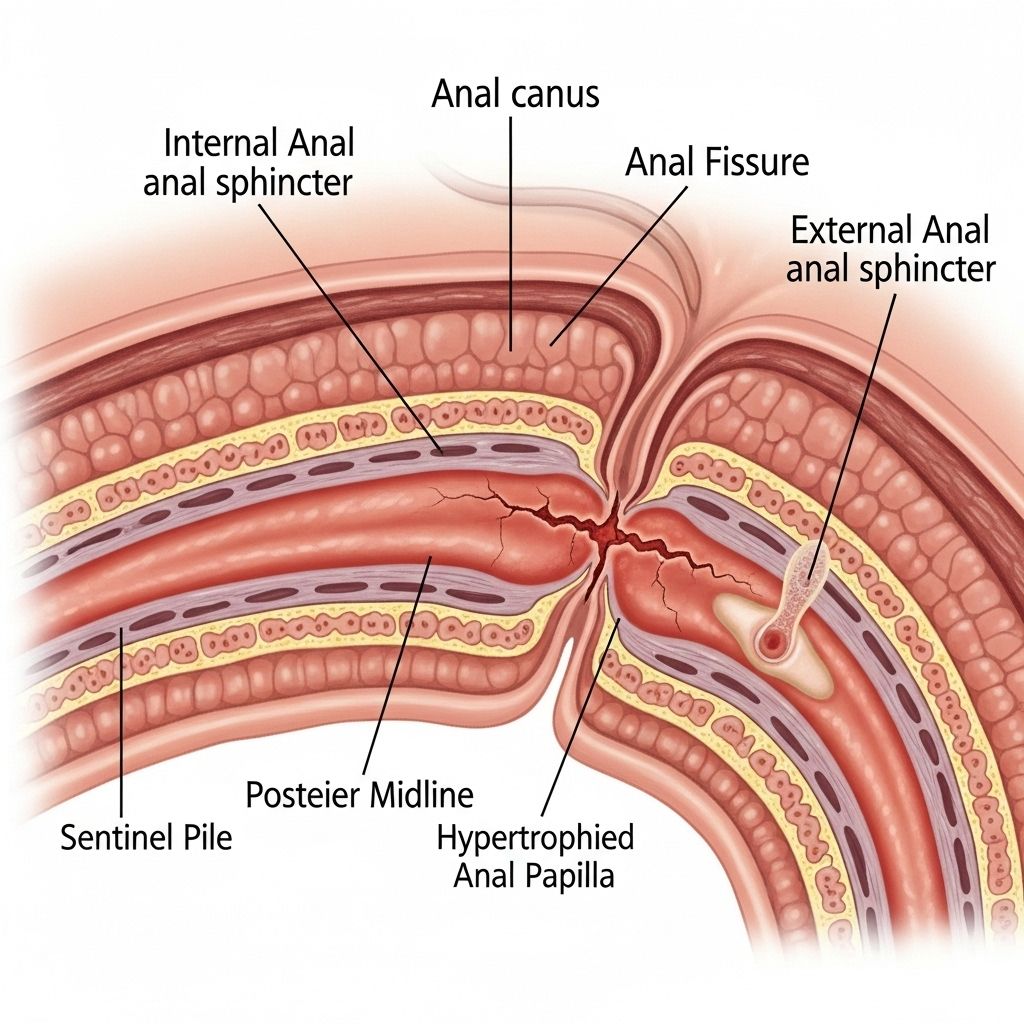
An anal fissure is a small tear in the thin, delicate tissue that lines the anus. This condition is common, affecting people of all ages—from infants to older adults—and is a frequent cause of anal pain and bleeding, especially during or after bowel movements.
Anal fissures can usually heal with simple treatments but may require medications or surgical intervention if persistent. This guide explores the causes, symptoms, diagnosis, prevention strategies, and all available treatment options for anal fissures.
What Is an Anal Fissure?
An anal fissure is a small crack or split in the anoderm, the moist lining of the lower anal canal. This tear is typically painful, especially when passing stool, and may cause bleeding or discomfort after defecation.
While most cases are short-lived and resolve on their own, some fissures can become chronic, lasting several weeks or longer, and may require more involved interventions.
Key Characteristics of Anal Fissures
- Small tear or ulcer in the lining of the anus
- Often causes severe pain and visible bleeding during bowel movements
- May be acute (short-term) or chronic (lasting more than 8 weeks)
- Can affect anyone, but appears more frequently in infants and adults aged 15–40
Symptoms of Anal Fissures
Symptoms vary in intensity but generally manifest during or after bowel movements. Common signs include:
- Pain during bowel movements
- Lingering pain after defecation, sometimes lasting for hours
- Bright red blood visible on toilet paper, stool surface, or in the toilet bowl
- Visible crack or ulceration in the skin around the anus
- Small lump or skin tag near the fissure site
Occasionally, individuals report spasms in the ring of muscle at the end of the anus (anal sphincter), which can exacerbate pain and delay healing.
When to Seek Medical Advice
- If pain during bowel movements or rectal bleeding persists for more than a few days
- If self-care measures do not provide relief within two weeks
- If symptoms interfere with daily activities or quality of life
Causes of Anal Fissures
Several factors can lead to the development of anal fissures. The majority of cases relate to trauma or irritation of the anal lining.
- Constipation: Straining and passing hard stools can tear the delicate tissue
- Diarrhea: Frequent or acidic stools can irritate and break down the lining
- Presence of a tight anal sphincter muscle (high resting tension)
- Inflammatory bowel diseases (IBD, Crohn’s disease, ulcerative colitis)
- Anal intercourse or local trauma
- Vaginal childbirth
- Infections (sexually transmitted infections like syphilis or herpes)
- Rarely, tumors or other underlying medical conditions
While constipation is especially common in children, adults may develop fissures through persistent diarrhea, IBD, or mechanical trauma. Pregnant women and new mothers are also at higher risk.
Diagnosis of Anal Fissures
A healthcare professional can diagnose anal fissures through a careful history and physical examination. Key aspects of diagnosis include:
- Visual inspection: The fissure appears as a linear tear in the anoderm, typically in the posterior midline of the anus
- Assessment for associated skin tags, sentinel pile, or hypertrophied papilla
- Presence of bleeding or granulation tissue
- Exclusion of other causes of rectal pain or bleeding (e.g., hemorrhoids, abscess, malignancy)
Further investigations—such as anoscopy or colonoscopy—may be recommended if symptoms are atypical, recurrent, or suggestive of more serious underlying disease.
Types of Anal Fissures
Anal fissures are categorized based on duration and location:
| Type | Duration | Features |
|---|---|---|
| Acute | < 6 weeks | Fresh tear, minimal scarring, generally resolves with self-care |
| Chronic | > 6–8 weeks | Persistent fissure, possible skin tags, hypertrophied papilla, may require medical/surgical intervention |
Most fissures occur in the posterior (back) midline of the anus, but anterior (front) fissures are possible, especially in women.
Prevention of Anal Fissures
Preventive strategies focus on minimizing factors that strain or irritate the anal canal. Effective measures include:
- Eating a high-fiber diet (whole grains, fruits, vegetables)
- Drinking plenty of fluids to keep stools soft
- Avoiding prolonged sitting or straining while defecating
- Maintaining good bowel habits and regular exercise
- Managing underlying medical conditions like IBS, IBD, or other sources of inflammation
By reducing constipation and diarrhea, most people can lower their risk of developing new fissures.
Treatment Options for Anal Fissures
Treatment depends on the duration (acute or chronic) and severity of symptoms. Initial management is usually conservative, progressing to medical or surgical approaches if needed.
Conservative (Self-Care) Approaches
- Sitz baths: Soaking the anal area in warm water (10–20 minutes, several times daily) helps relax the sphincter and relieves discomfort
- Stool softeners: Over-the-counter options (e.g., docusate) reduce stool hardness
- Dietary fiber: Increased fiber intake through foods or supplements (e.g., psyllium, Metamucil) makes stools easier to pass
- Pain relief: Topical anesthetic creams (lidocaine) for symptomatic relief
- Avoiding irritants: Gently cleaning the area, avoiding harsh soaps or wipes, and minimizing straining
Most acute fissures heal with these measures within 6 to 8 weeks. Conservative therapy works for more than 80% of affected individuals.
Medications
- Topical nitroglycerin (Rectiv): Increases blood flow and relaxes anal sphincter; may cause headaches
- Calcium channel blockers: Ointments (diltiazem, nifedipine) help relax muscles, promote healing
- Botulinum toxin (Botox) injection: Temporarily paralyzes the sphincter, allowing fissure to heal; benefits last 2–3 months
- Topical anesthetics: Lidocaine for pain management during bowel movements
Medical therapy is recommended if conservative methods fail, or for chronic fissures resistant to self-care. Some medications may have side effects (e.g., headache from nitroglycerin, transient incontinence from Botox or surgery).
Surgical Treatments
- Lateral internal sphincterotomy (LIS): The standard surgical approach for chronic, unresponsive fissures; a small part of the anal sphincter muscle is cut to relieve spasm, improve healing, and reduce pain
- Performed as a day surgery under anesthesia
- Efficacy: Surgery is significantly more effective than other treatments for chronic fissures but carries a small risk of fecal incontinence
- Recommended when other treatments fail or if symptoms are severe
Other procedures—such as injection of medications or use of creams—may be considered as alternatives for patients at higher risk of incontinence or where surgery may be contraindicated.
Complications and Risks
Untreated anal fissures can lead to chronic pain, persistent bleeding, secondary infections, or formation of skin tags and hypertrophied papillae. Long-standing fissures may predispose patients to anorectal abscesses or fistula formation.
Surgical treatment may cause rare complications including incontinence, infection, or recurrence of fissures.
Living with Anal Fissures
The psychological and physical impact of fissures can be considerable, affecting work productivity, social interactions, and daily comfort. Strategies for living well with fissures include:
- Partnering with healthcare professionals for ongoing management
- Adhering to prescribed dietary, hygiene, and medication regimens
- Minimizing stress and anxiety related to bowel habits
Most individuals recover fully with conservative or medical treatment, while surgery offers a reliable solution for chronic cases.
FAQs About Anal Fissures
Q: What causes anal fissures?
A: The primary causes are constipation, straining, passing hard stools, or frequent diarrhea. Trauma, childbirth, infections, and underlying conditions like IBD may also contribute.
Q: Are anal fissures contagious?
A: No, anal fissures are not contagious. They result from mechanical or chemical injury to the anoderm.
Q: How long does it take for an anal fissure to heal?
A: Most acute fissures heal within 6 to 8 weeks using conservative measures. Chronic fissures may persist and require medication or surgery.
Q: Can anal fissures lead to serious health problems?
A: While most fissures are benign, chronic cases may result in persistent pain, secondary infection, or in rare cases, anorectal abscess or fistula. Surgery is safe and effective for long-standing fissures, though carries minor risks of incontinence.
Q: What steps can I take to prevent anal fissures?
A: Maintain a high-fiber diet, stay hydrated, avoid straining, and practice good bowel habits. Managing underlying medical conditions can further reduce risk.
Frequently Asked Questions (FAQs)
Q: When should I see a doctor about anal fissures?
A: Seek medical attention if pain or bleeding persists beyond two weeks, conservative self-care is ineffective, or if symptoms are severe and interfering with daily life.
Q: Will I need surgery for an anal fissure?
A: Surgery is reserved for chronic fissures not responding to conservative and medical treatments. Most cases resolve without surgical intervention.
Q: What are the risks of surgery for anal fissures?
A: The main risk is minor incontinence, though this is rare. Infection, recurrence, and mild discomfort may also occur.
Summary Table: Anal Fissure Treatments
| Treatment | Approach | Effectiveness | Risks/Side Effects |
|---|---|---|---|
| Conservative | Sitz baths, fiber, hydration, stool softeners | High (80%) | Minimal |
| Medication | Nitroglycerin cream, calcium channel blockers, Botox, anesthetics | Moderate | Headache, irritation, transient incontinence |
| Surgery (LIS) | Sphincterotomy | Very high for chronic cases | Low risk of incontinence, infection |
Conclusion
Anal fissures are a common, painful condition that can affect anyone. Early recognition, adherence to conservative strategies such as a high-fiber diet and warm baths, and timely medical intervention are crucial for prompt healing. Chronic or complex fissures may need medication or surgical care. Partnership with healthcare providers can ensure effective treatment and minimize complications, supporting long-term comfort and digestive health.
Read full bio of medha deb