Chronic Kidney Disease (CKD): Symptoms, Stages, Diagnosis, and Treatment
Understand chronic kidney disease, its symptoms, causes, stages, and explore diagnostic methods, management, treatments, and living well with CKD.
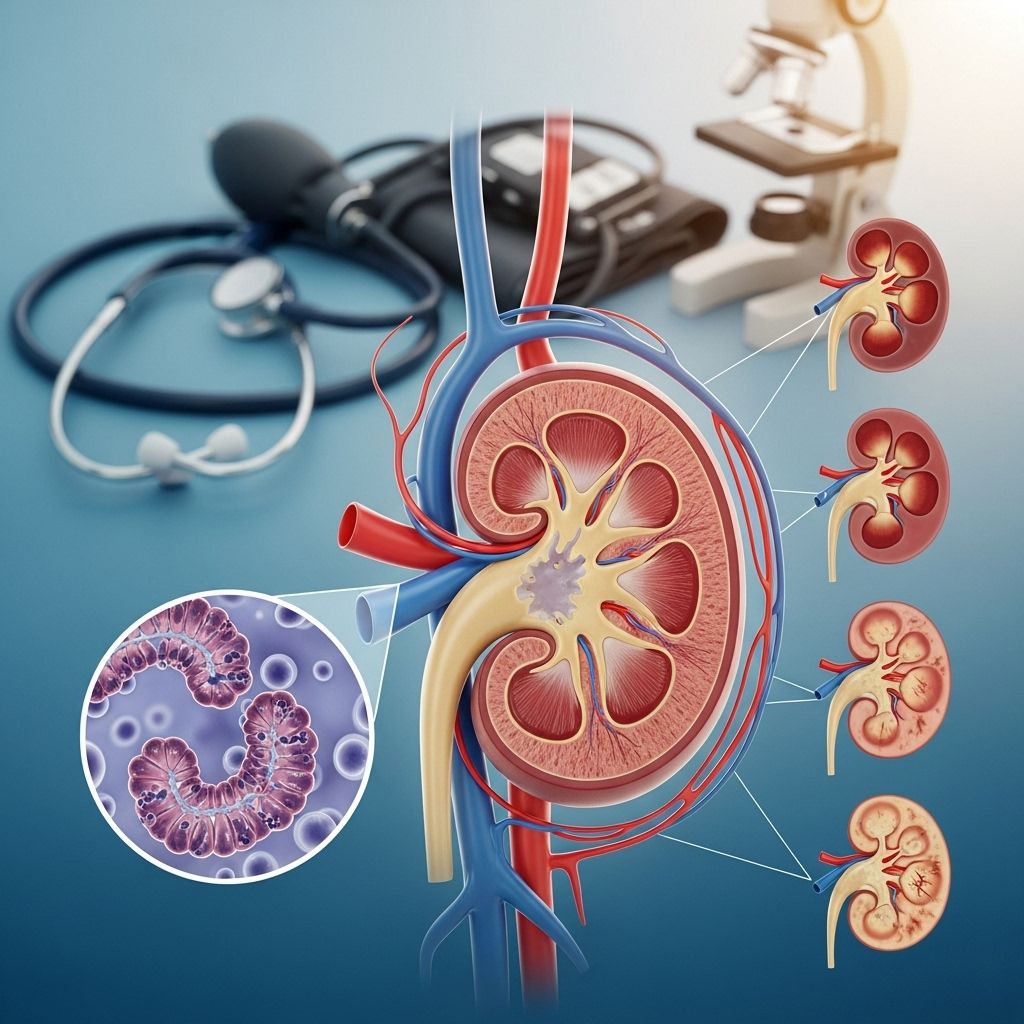
Chronic kidney disease (CKD) is a long-term condition in which the kidneys gradually lose function. Understanding CKD, its causes, symptoms, diagnosis, and treatment options is crucial for effective management and improved quality of life.
What is Chronic Kidney Disease?
Chronic kidney disease (CKD) refers to the progressive damage and reduced function of the kidneys, typically over several months or years. The kidneys are essential organs responsible for filtering waste products from the blood, regulating fluid and electrolyte balance, and managing blood pressure.
- CKD is often described as a silent condition because symptoms may not appear until the disease is at an advanced stage.
- CKD is not curable but can be managed to slow its progression and reduce the risk of complications.
Symptoms of CKD
Symptoms of chronic kidney disease often develop slowly and may not be noticeable until kidney function is significantly impaired. Early detection, therefore, is challenging.
- Fatigue and low energy
- Swelling in ankles, feet, or hands (oedema)
- Shortness of breath
- Nausea or vomiting
- Blood in the urine (haematuria)
- Persistent itching
- Muscle cramps
- Loss of appetite and unexplained weight loss
- Trouble sleeping (insomnia)
- Increased need to urinate, particularly at night
- Difficulty concentrating or memory problems
When to Seek Medical Advice
CKD is often detected from routine blood or urine tests. Consult a healthcare professional if you:
- Have symptoms of CKD
- Have risk factors such as diabetes, high blood pressure, heart disease, or a family history of kidney issues
- Notice changes in urination, foamy urine, or swelling in your arms or legs
Causes and Risk Factors of CKD
CKD can result from various conditions that damage the kidneys over time. The most common causes are:
- Diabetes (type 1 and type 2): persistently high blood sugar can damage kidney filters.
- High blood pressure (hypertension): increased pressure can damage the delicate kidney structures.
- Cardiovascular disease: diseases affecting blood vessels often impact the kidneys.
- Glomerulonephritis: group of diseases causing inflammation of kidney filters (glomeruli).
- Long-term blockage of the urinary tract: caused by enlarged prostate, kidney stones, or tumors.
- Recurrent kidney infections (pyelonephritis).
- Inherited conditions: such as polycystic kidney disease.
Risk Factors
- Older age
- Ethnic background (South Asian or African-Caribbean populations are at greater risk)
- Family history of kidney disease
- Obesity
- Smoking
- Prolonged use of certain medications (such as NSAIDs)
How CKD is Diagnosed
CKD is usually diagnosed using:
- Blood tests: to check kidney function by measuring levels of creatinine and calculating estimated glomerular filtration rate (eGFR).
- Urine tests (urinalysis): to check for protein (albumin) or blood in urine, indicating kidney damage.
- Blood pressure measurement: high blood pressure is both a cause and a consequence of CKD.
- Kidney imaging: ultrasound scans to assess size and structure.
- Kidney biopsy: rarely needed, but may be required if the cause of CKD is unclear.
Kidney Function Tests Explained
- eGFR (estimated glomerular filtration rate): indicates how well kidneys are filtering; measured in mL/min/1.73m².
- Urine albumin-to-creatinine ratio (ACR): detects protein leakage in the urine; a sign of kidney damage.
Stages of Chronic Kidney Disease
CKD is classified into five stages, based on eGFR results and evidence of kidney damage. Staging helps guide treatment and referral needs.
| Stage | eGFR (mL/min/1.73m²) | Description |
|---|---|---|
| 1 | ≥ 90 | Normal or high kidney function with evidence of damage (such as protein in urine) |
| 2 | 60-89 | Mild loss of kidney function, possible kidney damage |
| 3a | 45-59 | Mild to moderate loss of kidney function |
| 3b | 30-44 | Moderate to severe loss of kidney function |
| 4 | 15-29 | Severe loss of kidney function |
| 5 | < 15 (or dialysis) | Kidney failure, often requiring dialysis or transplant |
Potential Complications of CKD
CKD can lead to a number of complications, including:
- High blood pressure (hypertension)
- Anemia (low red blood cell count)
- Weak bones (osteodystrophy)
- Fluid retention, causing swelling and shortness of breath
- High levels of potassium in the blood (hyperkalemia)
- Increased risk of cardiovascular disease
- Uremic syndrome (buildup of toxins in the blood)
Treatment Options for Chronic Kidney Disease
There is no cure for CKD, but a combination of lifestyle changes, medications, and, in advanced cases, dialysis or kidney transplantation can help manage the condition and slow its progression.
Lifestyle Changes
- Eating a healthy, balanced diet low in salt and saturated fat
- Engaging in regular physical activity
- Maintaining a healthy weight
- Not smoking
- Limiting alcohol intake
- Managing blood sugar levels (if diabetic)
Medications
- Blood pressure-lowering medications (e.g., ACE inhibitors, ARBs): Protect kidney function and control blood pressure.
- Medicines to control diabetes if present.
- Statins to lower cholesterol and reduce heart disease risk.
- Phosphate binders for those with mineral imbalances.
- Diuretics (water tablets) to reduce fluid retention.
- Other medications as needed (for anemia, bone disease, etc.).
Monitoring and Regular Check-Ups
- Frequent blood and urine tests to assess kidney function and levels of important substances (e.g., potassium, phosphate).
- Blood pressure monitoring.
- Regular review of medications, especially if you have other conditions.
- Immunizations recommended to reduce risk of infections.
Advanced CKD Treatments
When kidney function drops below a critical level (usually eGFR < 15), advanced treatments are considered:
- Dialysis: Artificially removes waste products and excess fluid from the blood. Types include haemodialysis and peritoneal dialysis.
- Kidney Transplant: Surgically placing a healthy kidney from a donor. This offers the best long-term outcome for many people with kidney failure.
- Supportive (conservative) care: Focuses on managing symptoms and maintaining quality of life without dialysis or transplant, suitable for those for whom advanced CKD treatments are not appropriate.
Diet and Nutrition for CKD
Following a healthy diet is key for people with CKD. Depending on the stage and individual factors, dietary recommendations may include:
- Lowering salt (sodium) intake to help control blood pressure
- Managing protein intake (especially in later stages)
- Limiting foods high in potassium and phosphate
- Staying hydrated, but avoiding overconsumption of fluids if fluid retention is an issue
- Seeing a renal dietitian for personalized advice
Living Well With Chronic Kidney Disease
A CKD diagnosis can feel overwhelming, but with proper management, many people continue to live active lives. Strategies for coping with CKD include:
- Learning about CKD and its management
- Attending regular appointments and monitoring health
- Taking medications as prescribed
- Seeking support from healthcare teams, friends, and patient organizations
- Reporting new or worsening symptoms promptly
- Staying up to date with recommended vaccinations
Emotional Wellbeing
Coping with a long-term condition can impact your mental health.
- Discuss feelings of anxiety or depression with your GP or kidney care team
- Support groups and counseling can help manage stress and emotional challenges
Preventing CKD and Reducing Progression
- Maintain a healthy lifestyle: balanced nutrition, regular exercise, and a healthy weight
- Control blood pressure and blood sugar
- Limit alcohol and avoid tobacco use
- Take medications as prescribed and avoid overuse of NSAIDs
- Have regular blood and urine tests if you have risk factors or a family history
Frequently Asked Questions (FAQs)
What does chronic kidney disease mean?
Chronic kidney disease means the kidneys have sustained permanent damage, causing a gradual loss of function over time. The condition can range from mild to severe and often requires ongoing management.
Is chronic kidney disease curable?
CKD cannot be cured, but early detection, lifestyle changes, and medical management can slow progression and reduce complications.
Will I need dialysis?
Dialysis is only needed in advanced CKD (usually stage 5) when kidney function is extremely low and symptoms cannot be controlled by other means.
Can CKD be prevented?
Many cases can be prevented or their progression slowed by controlling risk factors such as hypertension, diabetes, and avoiding kidney-damaging medications.
Does diet affect CKD?
Diet is a crucial component in CKD management. A healthy, low-salt diet helps manage blood pressure and decreases strain on the kidneys; individualized advice is often provided by a renal dietitian.
Resources and Support
- Your GP and kidney care team
- Renal dietitians
- Patient support organizations (e.g., Kidney Care UK, National Kidney Federation)
- NHS online resources for kidney disease
For more detailed and personalized advice, consult your healthcare professional and consider accessing patient resources and support networks.
References
- https://www.ukkidney.org/health-professionals/information-resources/uk-eckd-guide
- https://www.nottsapc.nhs.uk/media/cz1jrhbu/guidelines-for-management-of-chronic-kidney-disease-ckd-for-adults.pdf
- https://www.plymouthhospitals.nhs.uk/display-pil/pil-your-guide-to-living-with-chronic-kidney-disease-7043/
- https://www.bartshealth.nhs.uk/download/how-to-look-after-your-kidneys.pdf?ver=52501
- https://www.nhs.uk/conditions/kidney-disease/
- https://www.nhs.uk/conditions/kidney-disease/treatment/
- https://www.worcsacute.nhs.uk/documents/documents/patient-information-leaflets-a-z/2684-a-guide-to-diet-and-chronic-kidney-disease/
- https://www.kidney.org.uk/healthy-eating-for-people-with-chronic-kidney-disease-ckd
- https://rightdecisions.scot.nhs.uk/m/2735/1087-adult-chronic-kidney-disease.pdf
Read full bio of medha deb