Horner Syndrome: Causes, Symptoms, Genetics, and Management
Uncover the rare neurological disorder that affects the eye and face, its origins, symptoms, and approaches to care.
What is Horner Syndrome?
Horner syndrome is an uncommon neurological condition that specifically affects one side of the face and the eye. It arises due to compromised function of certain sympathetic nerves, resulting in characteristic physical signs localized to the affected side. The syndrome is also known as Bernard-Horner syndrome, Oculosympathetic palsy, and Von Passow syndrome.
Key Features of Horner Syndrome
- Ptosis: Drooping of the upper eyelid on the affected side.
- Miosis: Constricted pupil unable to dilate properly.
- Anhidrosis: Reduced or absent sweating on part of the face.
- Enophthalmos: Sunken appearance of the eye (less commonly reported).
- Iris heterochromia (in children): Difference in iris color due to disrupted pigment development.
Frequency and Prevalence
It is estimated that about 1 in 6,250 babies are born with Horner syndrome. The rate at which the syndrome develops later in life (acquired Horner syndrome) is not precisely known, but overall the disorder is judged as uncommon in the general population. The congenital form (present at birth) accounts for approximately 5% of cases.
How Horner Syndrome Occurs: Causes and Pathways
The underlying mechanism of Horner syndrome is interruption or damage to the cervical sympathetic nerves—a division of the autonomic nervous system, specifically the sympathetic branch. These nerves regulate important involuntary functions such as pupil dilation, eyelid elevation, and sweating on the face.
Sympathetic Nerve Pathways Involved
There are three main nerve pathways from the brain to the face and eyes, and Horner syndrome can result from damage to any of them:
- First Order (Central): Nerves running from the hypothalamus in the brain, through the brain stem and spinal cord to the upper chest. Disruption may result from stroke, blood flow interruption to the brain stem, hypothalamus tumors, demyelinating diseases, or spinal cord lesions.
- Second Order (Preganglionic): Nerves extending from the upper chest to the top of the lungs and along the carotid artery in the neck. Tumors in the upper lung, chest surgery, or traumatic injury may affect this pathway.
- Third Order (Postganglionic): Nerves running from the neck to the middle ear and eye structures. Common causes affecting this path include carotid artery lesions, middle ear infections, skull injuries, and severe headaches.
Common Causes
- Trauma: Birth injury (especially during difficult delivery), accidental injury to the neck, chest, or base of the skull.
- Surgery: Procedures involving the head, neck, or upper chest.
- Tumors: Neuroblastoma (a childhood cancer affecting nerve tissues), lung tumors, or other masses compressing sympathetic nerves.
- Vascular Issues: Agenesis of the carotid artery (lack of development), carotid artery dissection (tearing of artery wall layers), or other issues reducing blood flow to the nerves.
- Migraines and Headaches: Symptoms may appear transiently during severe headaches and resolve as the headache subsides.
- Infections: Middle ear infections or other local infections.
In about 35%–40% of cases, there is no clear underlying cause, which are termed idiopathic Horner syndrome.
Childhood and Congenital Horner Syndrome
- Can result from nerve or carotid artery injury during birth.
- Associated with developmental defects of arteries (like agenesis of the carotid artery).
- Neuroblastoma may be underlying in some cases.
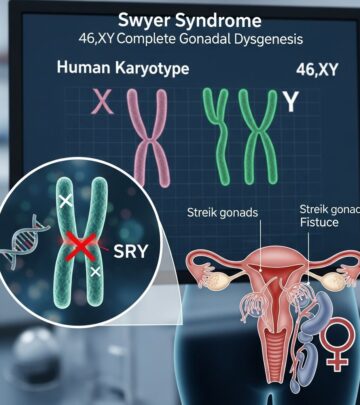
Genetic Aspects and Inheritance
Although congenital Horner syndrome can occasionally run in families, no specific genes have yet been identified as causing this disorder. Most cases are not inherited and are instead due to damage to nerves during birth or later life events. Very rare cases may show a pattern of autosomal dominant inheritance, meaning one altered copy of a gene could cause the disorder, though the responsible gene(s) remain unknown.
Genetic Terminology
- Autosomal Dominant: One copy of an altered gene in each cell is sufficient to cause the disorder.
- Idiopathic: No known cause or family history.
How Horner Syndrome Affects the Body
Disrupted sympathetic nerve function affects several processes:
- Pupil Dilation: Resulting in a persistently small pupil (miosis) on the affected side.
- Eyelid Control: Drooping of the upper eyelid (ptosis).
- Sweating: Reduced or absent facial sweating; may be limited to certain areas.
- Iris Pigmentation: In young children, lack of nerve stimulus can affect normal development, leading to heterochromia (different-colored eyes).
Symptoms are usually limited to one side of the face (unilateral), depending on the site of nerve damage.
Symptoms and Signs of Horner Syndrome
| Symptom/Sign | Description |
|---|---|
| Ptosis | Drooping upper eyelid |
| Miosis | Small (constricted) pupil |
| Anhidrosis | Decreased or absent sweating (one side of the face) |
| Iris Heterochromia (in congenital cases) | Difference in iris color between eyes |
| Enophthalmos | Sunken appearance of the eye (less common) |
These signs collectively help clinicians recognize the syndrome during examination. Symptoms usually do not cause pain but may cause visible facial asymmetry and impact vision in certain situations.
Similar Disorders and Differential Diagnosis
Other medical conditions present with symptoms similar to Horner syndrome and are important to consider during diagnosis:
- Adie Syndrome: Neurological disorder with abnormal pupil function, slow reaction to light.
- Wallenberg Syndrome: Neurological disorder caused by stroke or blood clot, may include Horner syndrome, speech difficulties, swallowing issues, dizziness, and sensory disturbances.
Frequently Used Alternative Names
- Bernard-Horner syndrome
- Oculosympathetic palsy
- Von Passow syndrome
- Horner’s syndrome
Diagnosis and Clinical Assessment
Diagnosing Horner syndrome involves:
- Physical examination of the eye and face.
- Clinical testing for pupil responses, eyelid contour, and sweating differences.
- Imaging studies (MRI, CT, ultrasound) to investigate underlying injuries, tumors, or vascular problems.
- Assessment of medical history, including recent trauma, surgeries, or neurological symptoms.
Further diagnostic workup may be required to rule out serious causes such as carotid artery dissection, neuroblastoma, or other masses, especially in children.
Patient Support and Advocacy Resources
- Genetic and Rare Diseases Information Center (GARD): Information on causes, research, and resources.
- Patient Support Organizations: Connect patients and families with support networks and advocacy groups.
- Clinical Trials: Opportunities for participation in clinical research investigating Horner syndrome.
- OMIM Catalog: Medical database containing catalog of genes and diseases even if no specific genes are linked to Horner syndrome yet.
- PubMed: Repository of scientific articles related to Horner syndrome for clinicians and researchers.
Frequently Asked Questions (FAQs)
Q: Is Horner syndrome inherited?
A: The vast majority of cases are not inherited and result from acquired nerve injury. Rare familial cases have been reported, but no specific genes are known to cause Horner syndrome.
Q: What causes Horner syndrome in newborns?
A: Newborns may develop the syndrome due to birth-related trauma, injuries to the cervical sympathetic nerves, or vascular defects like agenesis of the carotid artery. Rarely, neuroblastoma (childhood nerve tumor) may be involved.
Q: Can Horner syndrome disappear on its own?
A: If caused by transient factors such as a migraine or localized, reversible irritation, symptoms may resolve once the underlying issue is treated. Otherwise, persistent nerve damage usually means symptoms remain.
Q: Are males or females more affected?
A: Horner syndrome affects males and females equally; there is no known link to ethnicity or geographic location.
Q: What disorders are similar to Horner syndrome?
A: Adie syndrome (with pupil abnormalities) and Wallenberg syndrome (neurological syndrome, sometimes includes Horner’s symptoms) may present similarly, and should be ruled out during diagnosis.
Treatment and Management Approaches
Treatment of Horner syndrome depends on addressing the underlying cause:
- For reversible causes such as migraines or infections, treatment resolves symptoms.
- If trauma, surgery, or tumors are the cause, direct treatment (such as rehabilitation, surgery, or oncology care) is required.
- Congenital cases may require supportive eye care and regular monitoring for developmental issues or vision changes.
- No specific drugs cure Horner syndrome. Management focuses on underlying condition and symptomatic relief.
Patients and caregivers should seek a thorough evaluation to determine the cause, especially if symptoms occur suddenly, are accompanied by pain, or affect other body areas.
Additional Resources and References
- Scientific Articles on PubMed: Access recent research and clinical case reports.
- OMIM Genes and Diseases Catalog: For clinicians investigating other genetic or neurologic conditions.
- Genetic and Rare Diseases Information Center (GARD): Further informational support for patients.
- Patient Advocacy and Support: Organizations providing resources and connections for families and individuals living with Horner syndrome.
- Clinical Trials: Opportunities for participation in studies aiming to improve understanding and treatment options.
Conclusion
Horner syndrome is a rare disorder marked by characteristic symptoms due to sympathetic nerve disruption, most often arising through acquired injury, trauma, tumors, or vascular events. Although most cases are not genetic, rare familial patterns have been described. Accurate diagnosis, careful clinical assessment, and targeted treatment are essential. Educational and advocacy resources offer ongoing support for affected individuals and their families.
Read full bio of Sneha Tete