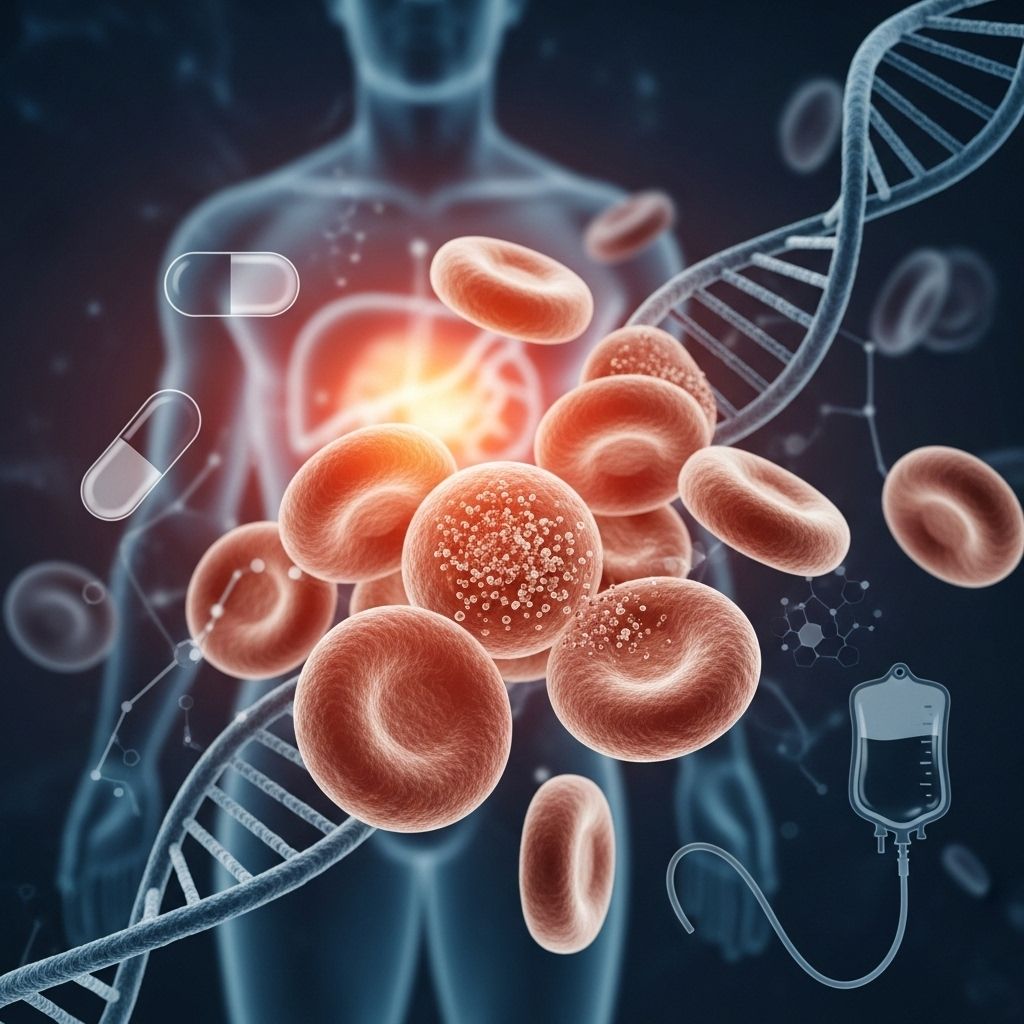
Hypochromic Microcytic Anemia with Iron Overload: Genetics, Symptoms, and Management
A rare inherited disorder combining impaired red blood cells and excessive liver iron accumulation due to genetic mutations.
Hypochromic Microcytic Anemia with Iron Overload
Hypochromic microcytic anemia with iron overload is a rare genetic disorder that impairs the normal transport of iron within cells. This impairment results in anemia—a shortage of functional red blood cells—alongside progressive accumulation of iron within the liver, which can eventually affect liver function.
Overview
- Anemia type: The affected red blood cells are microcytic (smaller than normal) and hypochromic (paler than normal) due to reduced hemoglobin content.
- Iron overload: Although iron is absorbed from the gut, red blood cells can’t utilize it efficiently. Excess iron accumulates in the liver, which may lead to liver disease as individuals mature.
- Onset: Anemia is typically apparent at birth, while iron overload symptoms intensify in adolescence or early adulthood.
- Frequency: Fewer than a dozen cases reported globally, indicating extreme rarity.
Description and Core Features
This disorder primarily disrupts iron metabolism and hemoglobin synthesis in the body, specifically affecting red blood cells and the liver. Iron, an essential component of hemoglobin, is required by red blood cells to carry oxygen throughout the body. In hypochromic microcytic anemia with iron overload, red blood cells cannot access or utilize iron, resulting in:
- Low red blood cell production (anemia)
- Production of abnormally small (microcytic) and pale (hypochromic) red blood cells
- Accumulation of unused iron in the liver over time (hepatic iron overload)
Common symptoms and signs include:
- Pallor (pale skin)
- Tiredness or fatigue
- Slow growth in affected children
Liver dysfunction may develop as excess iron builds up, typically manifesting in adolescence or early adulthood.
Frequency and Epidemiology
Hypochromic microcytic anemia with iron overload is considered extremely rare. Only a handful of families have been described in scientific literature, and case reports indicate its occurrence is likely limited to fewer than ten families worldwide.
Detailed Causes and Genetic Factors
The primary genetic cause of this disorder is mutation of the SLC11A2 gene, which encodes for the divalent metal transporter 1 (DMT1) protein.
Function of DMT1 Protein
- DMT1 is present in all tissues and transports positively charged iron ions within cells.
- In the small intestine (duodenum), DMT1 is located within microvilli and assists with iron absorption from food.
- In other cell types, including immature red blood cells (erythroblasts), DMT1 moves iron from cellular compartments into the cytoplasm, allowing its use for hemoglobin synthesis.
Effect of SLC11A2 Mutations
- More than seven pathogenic mutations have been detected, mostly altering single amino acids in the DMT1 protein.
- Mutant DMT1 leads to:
- Reduced production of the protein
- Decreased functional activity
- Impaired localization within cells
- In red blood cells, defective DMT1 results in insufficient iron available for hemoglobin synthesis, causing anemia.
- In the intestine, defective DMT1 would reduce absorption, but cells compensate by upregulating DMT1, paradoxically increasing iron absorption. However, this iron can’t be used by the red blood cells, leading to iron buildup in the liver.
- Other tissues remain largely unaffected due to alternative iron transport pathways.
Related Gene Names
- DCT1
- DMT1 (divalent metal transporter 1)
- NRAMP2 (Natural resistance-associated macrophage protein 2)
- Solute carrier family 11 member 2
Inheritance Pattern
This condition is inherited in an autosomal recessive manner. Individuals inherit two copies of the mutated SLC11A2 gene—from each parent. Parents are typically asymptomatic carriers, possessing only one copy of the faulty gene.
Inheritance Table
| Inheritance Type | Parent Genotype | Child Risk |
|---|---|---|
| Autosomal Recessive | Both parents are carriers (one mutated gene, one normal gene) | 25% chance affected, 50% chance carrier, 25% chance unaffected |
Clinical Features and Manifestations
- Blood and Forming Tissues:
- Anemia—observable from birth; low red blood cell count
- Microcytosis—smaller than normal red blood cells
- Hypochromia—lower hemoglobin content per cell leads to pale coloration
- Erythroid hyperplasia—increase in the production of immature red blood cells as compensation
- Metabolic and Digestive:
- Increased circulating iron concentration—blood iron levels elevated despite anemia
- Elevated hepatic iron concentration—iron accumulates in liver tissue, risking organ damage
Diagnosis
Diagnosis of hypochromic microcytic anemia with iron overload involves multiple steps:
- Clinical assessment of symptoms: anemia, fatigue, pallor
- Laboratory tests:
- Complete blood count (CBC) revealing low hemoglobin and microcytosis
- Serum iron studies showing slightly elevated to normal ferritin, high serum iron
- Liver function tests indicating iron overload or impaired function
- Genetic testing for mutations in the SLC11A2 gene
Available Genetic Testing Resources
Treatment and Management
Currently, as a rare and complex genetic disorder, standardized treatment protocols are limited. Management strategies generally aim to:
- Alleviate symptoms of anemia (may include blood transfusions)
- Monitor and address iron overload to prevent liver damage (liver monitoring, possibly chelation therapy)
- Routine follow-up in specialized centers experienced in rare genetic disorders
Ongoing research is needed to further guide therapeutic options, as only a few cases have been followed longitudinally.
Prognosis and Long-term Outlook
Patients with hypochromic microcytic anemia with iron overload:
- May have persistent anemia throughout life
- Face risk of progressive liver dysfunction due to accumulating iron
- Require ongoing monitoring for organ health, especially as symptoms can worsen during adolescence and young adulthood
Other Names for This Condition
- Microcytic anemia with hepatic iron overload
- Microcytic anemia with liver iron overload
- Anemia, hypochromic microcytic, with iron overload 1
Patient Support and Advocacy Resources
Several organizations offer information, advocacy, and genetic counseling:
- National Organization for Rare Disorders (NORD)
- Genetic and Rare Diseases Information Center
- MedlinePlus Genetics
Frequently Asked Questions (FAQs)
What is hypochromic microcytic anemia with iron overload?
This is a rare inherited disorder where the body cannot properly use iron for red blood cell production. Iron builds up in the liver, causing anemia and risking liver damage.
What causes this condition?
Mutations in the SLC11A2 gene, which encodes the DMT1 transporter protein, disrupt normal iron transport in cells.
What are the main symptoms?
Main symptoms include pale skin, chronic tiredness, slow growth in children, and eventually signs of liver impairment due to iron overload.
How is it inherited?
It is autosomal recessive: both parents must carry a mutated copy of the SLC11A2 gene for a child to be affected.
Can the iron overload affect other organs?
Primarily the liver is affected, because alternative iron transport routes limit damage in other tissues.
What treatments are available?
Treatment options focus on anemia management and reducing iron overload, but supportive care and regular monitoring are essential. Consultation at specialized genetic centers is recommended.
References and Further Reading
- MedlinePlus Genetics: Hypochromic microcytic anemia with iron overload
- Genetic Testing Registry
- National Organization for Rare Disorders (NORD)
- PubMed: SLC11A2 mutations and microcytic anemia
Summary Table: Key Facts about Hypochromic Microcytic Anemia with Iron Overload
| Feature | Details |
|---|---|
| Disorder Type | Inherited genetic anemia with liver iron overload |
| Main Gene | SLC11A2 |
| Inheritance | Autosomal recessive |
| Main Symptoms | Anemia, fatigue, pallor, slow growth, liver dysfunction |
| Onset | Birth (anemia); adolescence/early adulthood (liver symptoms) |
| Diagnosis | Blood tests, genetic testing, liver function evaluation |
| Treatment | Symptom management, monitoring iron levels, liver support |
| Other Names | Microcytic anemia with hepatic iron overload; DMT1 deficiency anemia |
FAQs at a Glance
- Q: Is hypochromic microcytic anemia with iron overload the same as hemochromatosis?
A: No. Traditional hemochromatosis features iron overload but lacks the marked microcytic, hypochromic anemia seen in this condition. - Q: Does iron supplementation help?
A: Iron supplements are not effective in this disorder, and can worsen iron overload. - Q: What is the difference from common anemia?
A: Most common anemia results from iron deficiency, whereas this genetic anemia results from defective iron utilization, not deficiency.
Read full bio of Sneha Tete