Swyer Syndrome (46,XY Complete Gonadal Dysgenesis): Genetics & Clinical Management
Understanding the genetic basis, symptoms, diagnosis, and treatment options for Swyer syndrome, a rare disorder of sex development.
Introduction to Swyer Syndrome
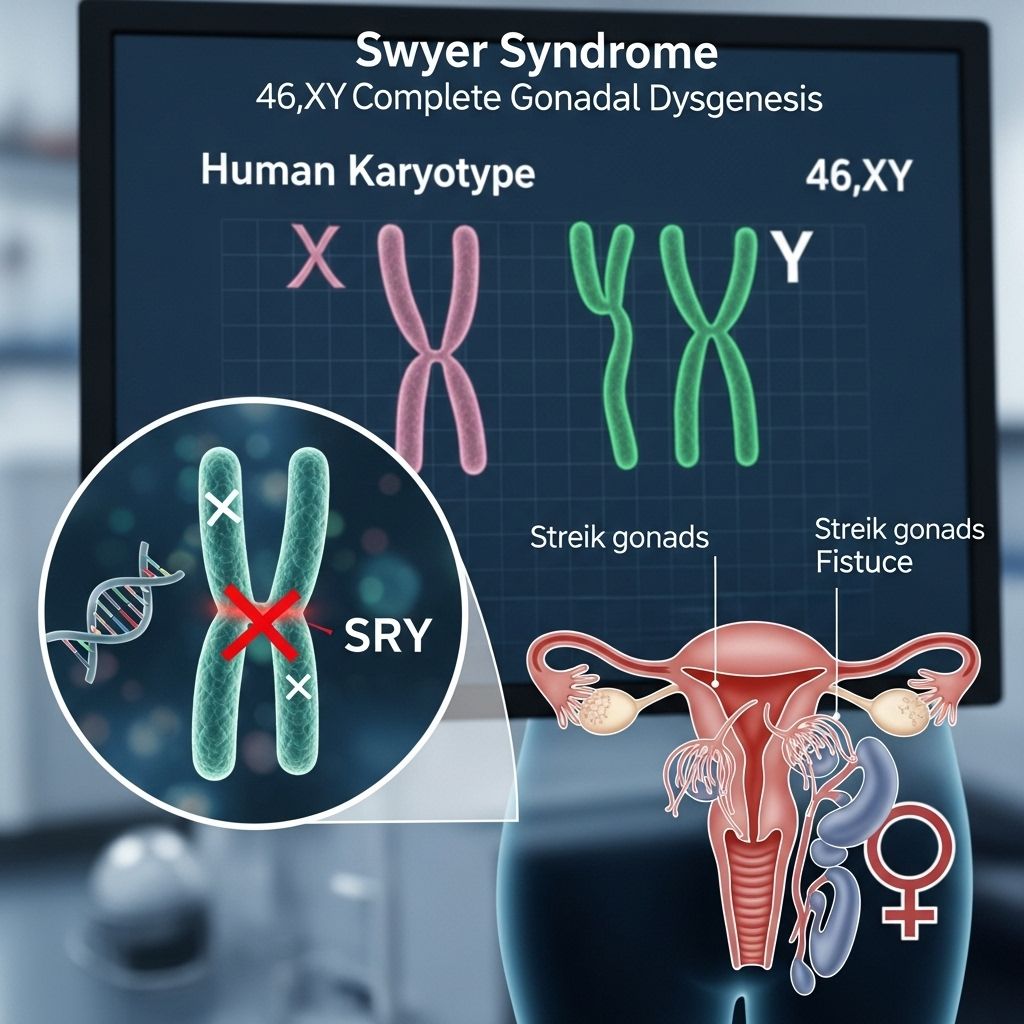
Swyer syndrome, also known as 46,XY complete (pure) gonadal dysgenesis, is a rare disorder of sex development (DSD) characterized by a 46,XY chromosomal pattern but female external genitalia and internal reproductive structures. Despite having typical male chromosomes, individuals with Swyer syndrome do not develop testes; instead, their gonads are underdeveloped and nonfunctional, referred to as ‘streak gonads.’ This condition is usually diagnosed when puberty fails to occur in adolescence, although some cases are identified earlier due to genetic testing or ambiguous genitalia at birth.
Genetic Basis and Causes
Sexual development in humans is typically guided by the presence of X and Y chromosomes. Girls and women usually have two X chromosomes (46,XX), and boys and men have one X and one Y chromosome (46,XY). In Swyer syndrome, individuals possess the 46,XY karyotype but develop female genitalia due to the absence of functional testes, which are normally responsible for producing male hormones that drive male physical development .
Gene Mutations in Swyer Syndrome
The development of testes requires the activation of several genes. The most well-known gene associated with Swyer syndrome is SRY (sex-determining region Y), located on the Y chromosome. The SRY gene initiates the cascade of events leading to testis formation. Mutations in the SRY gene prevent this process, resulting in the failure of testis development and the persistence of female anatomy . SRY gene mutations account for approximately 15–20% of Swyer syndrome cases.
However, Swyer syndrome can also be caused by mutations in other genes involved in sex development, including:
- MAP3K1: Associated with cases that are usually not inherited.
- NR5A1: Mutations can be inherited or occur spontaneously.
- DHH: Involved in rare inherited forms and follows an autosomal recessive pattern.
- CBX2, DMRT1/DMRT2, and others: Less common associations, with roles still being investigated .
| Gene | Chromosomal Location | Inheritance Pattern |
|---|---|---|
| SRY | Yp11.3 | Y-linked |
| MAP3K1 | 5q11.2 | Autosomal Dominant (usually sporadic) |
| NR5A1 | 9q33 | Autosomal Dominant (sex-limited) |
| DHH | 12q13.1 | Autosomal Recessive (sex-limited) |
Inheritance Patterns
Swyer syndrome can be inherited or arise spontaneously due to new (de novo) mutations:
- Y-linked inheritance: When caused by SRY gene mutations, the condition is Y-linked, meaning it is passed from father to son (only individuals with a Y chromosome can be affected) .
- Autosomal dominant inheritance: For genes like MAP3K1 and NR5A1, the condition can be inherited from either parent, but only affects those with a 46,XY karyotype (sex-limited). Many cases, however, are sporadic.
- Autosomal recessive inheritance: Mutations in DHH are inherited in a sex-limited autosomal recessive pattern, requiring two copies of the mutated gene (one from each parent) to manifest in an XY individual .
Symptoms and Clinical Presentation
Individuals with Swyer syndrome typically present with:
- Female external genitalia
- Normal uterus and fallopian tubes
- Underdeveloped streak gonads (nonfunctional gonadal tissue)
- Absence of ovarian function, leading to lack of puberty, breast development, and menstruation without hormonal therapy
Because the gonads do not produce sex hormones, affected individuals usually do not experience puberty. Without intervention, they may develop osteopenia or osteoporosis due to inadequate estrogen, which is important for bone health .
Diagnosis
Diagnosis of Swyer syndrome may occur at different stages:
- Before birth: Sometimes identified through prenatal genetic testing if there is a family history or atypical ultrasound findings.
- At birth: Rarely, if there are ambiguous genitalia.
- During adolescence: Most commonly, diagnosis occurs when a child does not go through puberty as expected.
The diagnostic process includes:
- Chromosomal analysis (karyotyping) to confirm 46,XY pattern
- Hormonal testing (low testosterone, elevated gonadotropins)
- Imaging studies (ultrasound, MRI) to evaluate internal reproductive structures and gonads
- Genetic testing to identify specific gene mutations
Treatment and Management
Hormone Replacement Therapy
Because individuals with Swyer syndrome do not produce estrogen or progesterone, hormone replacement therapy (HRT) is essential:
- Estrogen: Administered to induce puberty, breast development, and uterine growth. It is also crucial for bone health, reducing the risk of osteoporosis .
- Progesterone: Added later to regulate menstrual cycles, as the uterus would otherwise be exposed to unopposed estrogen, which can increase the risk of endometrial hyperplasia.
Gonadectomy
The streak gonads in Swyer syndrome have a significant risk of developing cancer, particularly gonadoblastoma. Therefore, surgical removal of the gonads (gonadectomy) is recommended, usually shortly after diagnosis, even in childhood .
Fertility Considerations
Individuals with Swyer syndrome do not produce eggs. However, if the uterus is present, pregnancy may be possible with assisted reproductive technology using a donated egg or embryo. Successful pregnancies have been reported in some cases .
Psychological and Social Support
Given the complexity of the diagnosis and potential impact on gender identity and fertility, psychological counseling and support are important components of comprehensive care.
Complications
The main complications associated with Swyer syndrome include:
- Infertility: Due to the absence of functional ovaries and eggs.
- Gonadal tumors: The risk of gonadoblastoma and other gonadal cancers is elevated, necessitating regular monitoring and early intervention.
- Osteoporosis: Without estrogen replacement, individuals are at risk for low bone density and fractures.
Frequently Asked Questions (FAQs)
What is the life expectancy for someone with Swyer syndrome?
With appropriate medical management—including hormone replacement therapy and removal of at-risk gonadal tissue—individuals with Swyer syndrome can expect a normal life expectancy. The main health concerns are related to hormone deficiency and cancer risk, both of which can be managed with modern therapies.
Can people with Swyer syndrome have children?
While individuals with Swyer syndrome do not produce eggs, pregnancy may be possible if they have a uterus and undergo assisted reproductive technology using donated eggs or embryos. Fertility options should be discussed with a specialist in reproductive endocrinology.
How is Swyer syndrome inherited?
Swyer syndrome can be inherited in several ways, depending on the causative gene. SRY-related cases are Y-linked, while other forms may follow autosomal dominant or recessive patterns. Many cases are due to new mutations and are not inherited.
Is Swyer syndrome the same as androgen insensitivity syndrome?
No. Swyer syndrome is characterized by underdeveloped gonads in a 46,XY individual with female external genitalia. Androgen insensitivity syndrome (AIS) occurs when the body does not respond to androgens (male hormones) despite having typical male chromosomes and functioning testes.
When is Swyer syndrome usually diagnosed?
Most individuals are diagnosed in adolescence when puberty fails to occur. Rarely, diagnosis happens at birth if there are ambiguous genitalia or before birth with prenatal genetic testing.
Living with Swyer Syndrome
Living with Swyer syndrome involves lifelong medical management, including hormone replacement therapy and regular follow-up to monitor for complications such as osteoporosis and cancer risk. Access to psychological support and reproductive counseling is also important for overall well-being.
Research and Future Directions
Ongoing research aims to better understand the genetic and molecular mechanisms underlying Swyer syndrome, as well as to improve diagnostic tools and reproductive options for affected individuals. Advances in assisted reproductive technology and hormone delivery systems continue to enhance quality of life and reproductive possibilities.
Conclusion
Swyer syndrome is a rare but important example of how disruptions in gene function can profoundly affect sexual development. With early diagnosis, appropriate hormone replacement, and preventive surgery, individuals with Swyer syndrome can lead healthy, fulfilling lives. Continued research and multidisciplinary care are essential to address the medical, psychological, and reproductive needs of affected individuals.
Read full bio of Sneha Tete












